
Psychedelic-Assisted Therapy, An Interview with Dr. Craig Heacock, MD
An interview with Dr. Craig Heacock, M.D., about innovative treatments in psychiatry. Curt and Katie talk with Dr. Heacock about psychedelic-assisted therapy – looking at efficacy, safety, and risks for these promising treatments (ketamine, psilocybin, and MDMA) for depression and trauma. We also discuss the debate about medicalization versus legalization of these substances.
It’s time to reimagine therapy and what it means to be a therapist. To support you as a whole person and a therapist, your hosts, Curt Widhalm and Katie Vernoy talk about how to approach the role of therapist in the modern age.
Click here to scroll to the podcast transcript.Transcript
Interview with Dr. Craig Heacock, M.D.
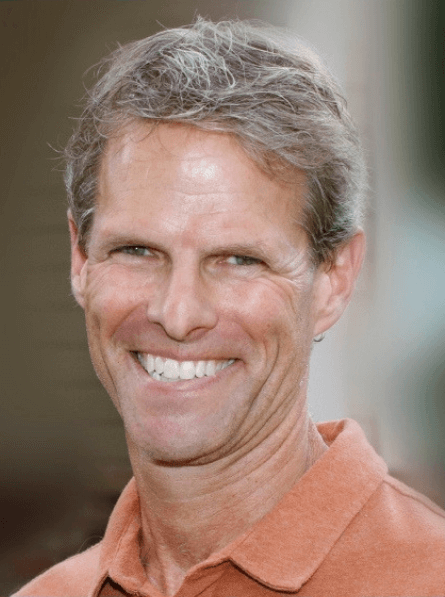 Dr. Craig Heacock is an adolescent/adult psychiatrist and addiction specialist in Colorado as well as the co-producer and host of the psychiatric storytelling podcast Back from the Abyss. He was a therapist in the Phase 3 trial of MDMA-Assisted Psychotherapy for PTSD and has particular interest in the use of ketamine and other psychedelics to treat severe mood disorders and PTSD. He is a graduate of the University of New Mexico School of Medicine and did his psychiatry training at Brown University.
Dr. Craig Heacock is an adolescent/adult psychiatrist and addiction specialist in Colorado as well as the co-producer and host of the psychiatric storytelling podcast Back from the Abyss. He was a therapist in the Phase 3 trial of MDMA-Assisted Psychotherapy for PTSD and has particular interest in the use of ketamine and other psychedelics to treat severe mood disorders and PTSD. He is a graduate of the University of New Mexico School of Medicine and did his psychiatry training at Brown University.
In this episode we talk about psychedelic-assisted therapy:
- The innovations in psychedelic-assisted therapy
- Why it is so hard to find a good psychiatrist, especially one that goes beyond med checks
- How psychiatry is changing, as well as how little has changed in medication since 1994
- Treatment-resistant may mean deep-seated trauma
- Definitions of psychedelics, psychedelic-assisted treatment
“Psychedelics [are] chemicals that take people deeply into other states, other parts of their conscious or unconscious and help them sort of plumb the psyche in a way that they’re not able to do without these substances.” – Dr. Craig Heacock
- Ketamine, MDMA, psilocybin
- Efficacy for treatment with ketamine, MDMA, psilocybin for trauma and depression
- The speed of building trust and moving into the working phase with these treatments
“It’s not that these treatments are replacing psychotherapy. In fact, I think it’s going to make psychotherapy even more thrilling because you can get through that tough slog of trying to break down the barriers and the defenses…and get to the real stuff so that work can actually happen.” — Dr. Craig Heacock, M.D. ⠀
- Safety concerns and side effects with ketamine, psilocybin, and MDMA
- Boundaries and safety for therapists (as well as clients) during these treatments
- The vulnerability during these treatments
- Self-assessment for mental health providers whether they should work in this space
- The importance of doing your own psychedelic treatment before being a therapist in this work
- Client-perceptions of clinicians doing their own psychedelic work (or publicly owning their story)
- The increasing acceptance of these types of treatments – the treatments becoming more mainstream
- Psilocybin – in trials for FDA approval for trauma treatment, but may be legalized before it is medicalized and used for treatment
- Medicalization versus legalization conversation
- The problems with medical THC (including making symptoms worse and psychotic breaks)
- Micro-dosing efficacy and risks and whether they should be managed by a doctor
- The importance of assessing sleep and substance use/abuse
- Abyss stories – how Dr. Heacock started telling these stories and the power of these stories
Our Generous Sponsors for this episode of the Modern Therapist’s Survival Guide:
Productive Therapist
You should be able to change the world and love your life. Productive Therapist can help you save time, make more money and feel a sense of relief. They provide mental health virtual assistants, business coaching, and unique training & support programs. Delegation can be the key to your freedom, but it is tough and comes with a learning curve. The Delegation Pro course will speed up that process by walking you through the important things you need to learn to start delegating like a pro (or a master)! You will get guidance on figuring out what tasks you should delegate, how to find the right person for the job and recommendations for the technology to make it a smooth process. As a listener of the Modern Therapist’s Survival Guide, you can get this course free by using the coupon code MODERN. Visit https://productivetherapist.teachable.com/p/delegation-pro to learn more.
Mulberry Web Design
Mulberry is a creative studio known for building fabulous custom websites, reasonable rates, and an obsessive dedication to customer service. The friendly team at Mulberry can take your private practice website to the next level with a complete redesign or help with your current website. Mulberry is a perfect fit for modern therapists ready to improve their online business presence. As a special welcome to listeners of this podcast, Mulberry is offering a 10% discount (up to $250!) on any service they provide. Mention the Modern Therapist’s Survival Guide podcast to receive your welcome discount.
Visit Mulberry at MulberryWebDesign.com today.
Resources for Modern Therapists mentioned in this Podcast Episode:
We’ve pulled together resources mentioned in this episode and put together some handy-dandy links. Please note that some of the links below may be affiliate links, so if you purchase after clicking below, we may get a little bit of cash in our pockets. We thank you in advance!
Laura Northrup Inside Eyes Podcast
Relevant Episodes of MTSG Podcast:
Therapists Struggling with Darkness
Who we are:
 Curt Widhalm, LMFT
Curt Widhalm, LMFT
Curt Widhalm is in private practice in the Los Angeles area. He is the cofounder of the Therapy Reimagined conference, an Adjunct Professor at Pepperdine University and CSUN, a former Subject Matter Expert for the California Board of Behavioral Sciences, former CFO of the California Association of Marriage and Family Therapists, and a loving husband and father. He is 1/2 great person, 1/2 provocateur, and 1/2 geek, in that order. He dabbles in the dark art of making “dad jokes” and usually has a half-empty cup of coffee somewhere nearby. Learn more at: http://www.curtwidhalm.com
 Katie Vernoy, LMFT
Katie Vernoy, LMFT
Katie Vernoy is a Licensed Marriage and Family Therapist, coach, and consultant supporting leaders, visionaries, executives, and helping professionals to create sustainable careers. Katie, with Curt, has developed workshops and a conference, Therapy Reimagined, to support therapists navigating through the modern challenges of this profession. In her spare time, Katie is secretly siphoning off Curt’s youthful energy, so that she can take over the world. Learn more at: http://www.katievernoy.com
A Quick Note:
Our opinions are our own. We are only speaking for ourselves – except when we speak for each other, or over each other. We’re working on it.
Our guests are also only speaking for themselves and have their own opinions. We aren’t trying to take their voice, and no one speaks for us either. Mostly because they don’t want to, but hey.
Stay in Touch with Curt, Katie, and the whole Therapy Reimagined #TherapyMovement:
Consultation services with Curt Widhalm or Katie Vernoy:
Connect with the Modern Therapist Community:
Our Facebook Group – The Modern Therapists Group
—
Get Notified About Therapy Reimagined Conferences
Modern Therapist’s Survival Guide Creative Credits:
Voice Over by DW McCann https://www.facebook.com/McCannDW/
Music by Crystal Grooms Mangano https://groomsymusic.com/
Transcript for this episode of the Modern Therapist’s Survival Guide podcast (Autogenerated):
Transcripts do not include advertisements just a reference to the advertising break (as such timing does not account for advertisements).
… 0:00
(Opening Advertisement)
Announcer 0:00
You’re listening to the Modern Therapist’s Survival Guide where therapists live, breathe and practice as human beings. To support you as a whole person and a therapist, here are your hosts, Curt Widhalm and Katie Vernoy.
Curt Widhalm 0:15
Welcome back modern therapists. This is the Modern Therapist’s Survival Guide. I’m Curt Widhalm, with Katie Vernoy. And one of the topics that our listeners have been asking for for quite a while is about the revolution of micro dosing and psychedelic assisted psychotherapy. And we have kind of been listening and trying to find a way to bring this topic to you. And today we’re joined by Dr. Craig Heacock. He’s a psychiatrist in Colorado and host of the Back from the Abyss podcast, who’s here to talk to us about the ways that this is showing really promising research into the mental health world as well as ways that clinicians should conceptualize this and maybe incorporate this and I feel obligated to say that we are not, at least Katie and I are not microdosing ahead of recording this episode. And we’ll actually have a relevant points a little bit later here. But thank you very much for joining us today. Dr. Heacock.
Dr. Craig Heacock 1:18
Thank you.
Katie Vernoy 1:19
We are so glad to have you here. I’ve been excited to talk about this topic for a while because I’ve been hearing so much about it. But before we dive in, we love to ask each of our guests: Who are you and what are you putting out into the world?
Dr. Craig Heacock 1:36
Well, I’m an adolescent being an adult psychiatrist in Colorado, and addiction specialist. I guess most recently, what I’ve been putting out into the world is my podcast. The last a year and a half I’ve been publishing, producing a psychiatric storytelling podcast called Back from the abyss. And also I have a huge interest in psychedelics and psychedelic assisted therapy and I do a lot of ketamine work. I’ve done about 1500 intramuscular and intravenous ketamine sessions. And just a couple of months ago, Lisa Ling did a documentary on psychedelic healing. And she for that documentary, she came to my office and filmed me doing some ketamine work. So she followed three different people, one doing MDMA work, one doing psilocybin one doing ketamine. So I think a lot of people saw that work, and is really excited and got inquiries from all over the country like, what is this ketamine thing? And what is ketamine assisted psychotherapy? And is this for me? And is this good for trauma? So I’m very interested in that realm.
Curt Widhalm 2:28
From a treatment standpoint, it’s really hard to find a good psychiatrist. And we know that the crisis in the mental health field is partially based on the absence of good psychiatrists. We’ve seen this across the country in a lot of different ways. The psychiatrists that I do find myself working with don’t seem to be falling into the same kind of patterns that I did see in the early parts of my career, where it was just a lot of medication management, med check sort of visits. That seems to be taking a little bit more of a holistic approach, and maybe not as much of a westernized medicine approach. How do you see psychiatry changing? And why is it so damn hard to find a good psychiatrist?
Dr. Craig Heacock 3:13
Yeah, well, those are two two separate questions. Let me just first speak to the why it’s so hard to find one. I just did a mini episode on this on Back from the Abyss. And the way I conceptualize it is, I talked about it, almost like salmon spawning home. That for a salmon to get back up river, it has to get up fish ladders and dams and escape the Grizzlies and the fishermen and very few make it back. And I think that’s a lot like psychiatry. So what I mean by that is the barriers to entry are huge. So to get into medical school is obviously very difficult, but they’re not really looking for psychiatrist kind of people. Like if you look at most people that go into medicine, they’re very, they’re very sciency. And they’re not necessarily psychologically minded. They’re not people, I think that necessarily done much therapy. They’re not necessarily people that have a lot of curiosity of the psyche, or the unconscious. So I argued in that episode, that there’s a bias against picking people who would be interested in psychiatry from the get go. And then when you get to medical school, there’s a definite anti psychiatry bias that still persists. It’s kind of it’s like, I feel like it’s a little bit like coming out gay, like when I finally confessed it, telling people it’s gonna be a psychiatrist, there was a lot of crap. And I’ve talked to some current medical students, and they say, yeah, it’s still something that you keep on the DL, because a lot of specialists are like, Oh, you’re not going to be a real doctor, or we’re giving you all this medical training, and you’re going to work with this weird black box called the psyche. But even for the people who make it through all that and get to psychiatry residency, I think and this was true for me, I think we don’t in all of this therapists and doctors don’t really know what we’re getting into until we dive in. But working with severe mental illness is really hard. And I know a bunch of my psychiatry colleagues who have moved to consultation, have moved to sort of the worried well. Practices have moved to very, very part time, who do a little impatient, who do locum tenens, but they don’t really see the outpatient psychiatry day in, day out year in year out people because it’s really hard. It’s really grueling work. And then the final thing is there’s this huge and Curt, you alluded to this, there’s this really difficult choice that psychiatrists have to make, which is, do we want to be med check people? Or do we want to be holistic. So it’s almost like in residency, we get trained to be garden consultants, we learn fertilizing and soils and plant selection and weeding and gardening and all that. But then we get out, we realize what the market really wants, they want fertilizer managers, you know, that’s what you want to get an employed job as a psychiatrist with a nice 401k and everything paid for a nice salary, they want you to do med checks, they want you to be a fertilizer manager. But if you want to be a holistic psychiatrist, you have to go on your own. And if you have to go on your own, then you have to decide am I going to take insurance or not? And then that’s basically this other difficult thing, where if you’re going to take insurance, you’re probably going to end up doing a lot of fertilizer management. And then at the very end, I think, are people who are trying to do what I’m doing, which is trying to do see whole person psychiatry, trying to give people the time they need and deserve. And the sad reality of psychiatry is, the vast majority of us who do this don’t take insurance because A: it’s a hassle, and B: we don’t have to. So then again, like in America, you know, the people with the money get the best of everything. And that’s true in psychiatry, for sure, but more than any other part of medicine. And it’s a shame. It’s so sad. And it’s one of the many reasons I started the podcast was just put some information and hope out there, because I know a lot of people can’t find a good psychiatrist. So, I thought, let’s just share some stories of hope and wisdom, and maybe that can help some people.
Curt Widhalm 6:48
I feel like one of us has to make the comment that with this whole fertilizer analogy. It’s just a lot of crap.
Dr. Craig Heacock 6:57
Yeah, well, that’s actually. So that leads into your second question, Curt, which is How is psychiatry changing? You know, I would argue that there’s been nothing really good in psychiatry since 1994. So, that’s when Lamotrigine came on the market. So since then, we’ve had atypical antipsychotics like Latuda, Abilify and Seroquel. And we’ve had TMS, which is a whole other topic, but really like what has actually meaningfully changed in psychiatry in 26 years? Nothing. We’ve come up with some new treatments, a lot of which are pretty toxic. But then in the last couple years, it’s just it’s never been a more thrilling time because these things are coming online like ketamine, psilocybin is coming soon, MDMA is almost surely coming soon. I mean, treatments that can actually transform people not just manage symptoms. And, and I think that’s also coming along with this realization that it’s so much of what’s treatment resistant in psychiatry, mental health is trauma. You know, for the longest time, you know, what psychiatry has not been able to help us people with deep trauma and people with negative symptoms of schizophrenia. And I don’t even really remember much PTSD training in my residency. And we never talked about anything somatic. Like the body didn’t exist was all the mind and the psyche. We did tons of psychodynamic exploration. But but now, I think coming on board with with psychedelics coming online, is this realization that oh, yeah, the body does keep the score, that trauma is held in the body spirit interface. That these treatment resistant people, why are they treatment resistant? A lot of them because they have trauma. Yeah, they’re depressed or they are anxious or panicky, but really what’s going on as they have these deep wells of often attachment trauma and neglect trauma. And so it’s really cool that as we’re realizing how much the body holds trauma and how much that’s expressing itself psychiatrically. That we’re actually now getting some tools where we can plumb the unconscious and get there. It’s never been a more exciting time, I think to be in doing trauma work in psychiatry.
Katie Vernoy 9:01
Yeah. I mean, it seems like there’s been this like psychedelic revolution that’s happening in psychiatry recently. Although it does seem a little quiet, but it’s still happening. And so for folks who aren’t aware of what’s going on, what is what is psychedelic assisted treatment, and and why is it happening now?
Dr. Craig Heacock 9:21
First of all, I think we have to talk about words. So, the word psychedelic means mind manifesting. And it’s an old term. So it’s kind of a general term. So psychedelics is a big tent. So is MDMA a psychedelic? I mean, most people would say no, they call it empathogenic . But so there’s a lot of, we have to be careful about words. But I think in general, when we’re talking about psychedelics, we’re talking about chemicals that take people deeply into other states, other parts of their conscious or unconscious and help them sort of plumb the psyche in a way that they’re not able to do without these substances. And so, right now what’s most relevant in psychiatry is ketamine. And ketamine is a dissociative general anesthetic that’s been around for 50 years. But in the last few years has become more and more become the go to treatment for suicidality, severe depression and PTSD. In my office, I’m doing probably 16 intravenous high dose treatments a week. It’s cool. It’s like being a shaman. Yeah, in fact, someone texted me the today and said, You fix my brain, you Shaman. And it’s cool. Ketamine is not fix. I think that’s important to note, Ketamine is a very powerful, psychedelic experience that for reasons we sort of understand and sort of don’t, is profound treatment that pulls people out of depression, often within 12 hours, but it’s not a fix. MDMA, what was formerly known as ecstasy looks like, it’s gotta be a fix for a lot of people. And we’re seeing, I worked in the MAPS MDMA study for three years. And we’re seeing people go into full remission from decades of PTSD, with just three, three, MDMA sessions plus integration and preparation. So I think of these, what I think of the role of these, these substances as speeding up that initial trust, and plumbing the depths of the trauma. That, you know, trauma work can take years. I mean, some trauma, some trauma treatments, the first three, four or five years of just about building trust, and MDMA can do that in 45 minutes, maybe, well, maybe an hour and 15 minutes. You know, psilocybin can take you to the depths of your unconscious, you know, within an hour and 15 minutes, places that you didn’t even know existed. So it’s not that these treatments are replacing psychotherapy. In fact, I think it’s going to make psychotherapy even more thrilling, because you can get through that tough slog of trying to break down the the barriers and the defenses and the defender parts and the dissociative, numbing and get to the real stuff, like break the dam, get it, get it all out so the work can actually happen. So, because trauma work can take years, and it’s so expensive. And, you know, a lot of people just cannot afford that. But I see these substances as being able to, again, bring people quickly to a place where they can start to do their trauma work and thrilling for therapists to be able to skip these really painful painful early months and months of months of years of just trying to build trust and, and collaboration.
… 12:33
(Advertisement Break)
Curt Widhalm 12:33
And speaking a lot to the benefits of these kinds of treatments; what kind of safety concerns might there be for patients and also for clinicians who are working with patients who are going through this kind of treatment?
Dr. Craig Heacock 12:46
I think we have to talk about each substance because a lot of ways saying psychedelics it’s like saying drugs or food, food is bad.
Curt Widhalm 12:53
It’s not just a candy bowl of ecstasy sitting in the waiting room.
Dr. Craig Heacock 12:58
Yeah, so I’ll just speak to Well, let me just talk about ketamine. Because ketamine, there’s hundreds of thousands of ketamine treatments occurring all over the country right now it’s saving people’s lives right now. Ketamine can make people extremely nauseated, get make them motion sick, it can be scary, it can raise your blood pressure. So we need to carefully manage those. It can make you manic, if you’re bipolar one, and you go a little too high on the dose, you can make people manic, I’ve seen that. Or and this, this actually ties in the bigger concern of psychedelic therapy in general. So when people are in an altered state, they’re very vulnerable there. And all sorts of dynamics can come up. So what a lot of clinicians are worried about is sexual boundary crossing, physical boundary crossing, and making sure that in this altered psychedelic space, that patients are safe, and that therapists are safe. So a year ago, I had a patient accuse me of sexually assaulting her during the ketamine session. And thank goodness that I have a medical assistant who’s with me the whole time. And she’s in the room. In fact, she’s the one that mostly monitors the IVs. I do the pre and post work. And it was a really powerful wake up call to this whole idea that when you’re working people that altered states, not only are they vulnerable, but you are vulnerable. And so I think what’s going to need to happen is either A: having two therapists in the room, having psychedelic sessions videotaped, again, not just for the patient’s protection, but for the therapist. And because these are such powerful chemicals, they also have this serious kind of boundary crossing boundary violation side. And that that has happened a lot in psychedelic work. It will continue to happen. I think in the biggest sense that’s my number one concern. I mean, yes, mushrooms can give you a really scary panic attack and yes, too much MDMA can cause serotonin syndrome but really like what’s the big risk? I think the big risk is that the psychedelic space is so vulnerable. Laura Northrup on her outstanding podcast, Inside Eyes, she talks a lot about this. This whole idea of entheogens and psychedelics being profound tools to heal sexual trauma. But without really careful monitoring, the therapists in even unknown like, these aren’t like predator therapists just to be in that kind of space with someone who’s so vulnerable therapists can unknowingly unwittingly get pulled into some into the role of the abuser and recreate the abuse during a psychedelic session.
Katie Vernoy 15:29
That feels like it’s something that’s pretty intense both for the patient, although they’re altered, but also for the therapist. To me, it seems like there may be some self assessment for folks who are interested in working in this space. What do you think it would take for someone to, to jump into this? Obviously, I also want to talk about like, what would non-psychiatrists do in the space because I’ve got colleagues are like, I really want to work on this. But for folks who are interested in this, it feels like there is, you know, it’s exciting, there’s there’s movement, but there’s also this huge vulnerability and, and it’s brand new territory. So who should be doing this? And who shouldn’t?
Dr. Craig Heacock 16:14
Yeah, so that’s a really good question. So first of all, I think, you know, there’s psychedelic work, if you will, or experiences that where people have a sitter just to keep them safe to keep them for like running out into traffic or something bad happening. And that’s fine and good. But that’s not a good idea for people with real trauma. So I think anybody who’s using these substances, whether it’s ketamine, MDMA, psilocybin, who has real trauma they need, in my opinion, a, an experienced therapist. So first is people I have a lot of people ask me, I want to be a psychedelic therapist. And what I tell them first is become a good therapist, do your own work, and then you’re going to need to do some psychedelic work, because I can’t imagine that you could effectively work with somebody in a psilocybin experience, if you hadn’t had that yourself. In the MAPS training, all the therapists are offered an all day MDMA experience so they can go through what the what the participants do. There’s an interesting controversy in the ketamine world. And it kind of breaks down between psychiatrists and anesthesiologists, which is, if you’re going to get people ketamine, should you have experienced it yourself and the anesthesiologist is like no, no; and psychiatrists would say, Oh, yeah, for sure. And I’ve been in online argument about that recently at a conference. And it really broke down between the anesthesiologist and the psychiatrist. But these are really powerful states. And I think that’s going to be one of the many things that you need to check your box, you are competent therapist, you, you have done your own work, you understand your own potential boundary crossing violation tendencies, and you’ve worked with that substance so you are familiar with it.
Curt Widhalm 17:53
On this debate on whether or not people should use it, going back to the comment that I made in introducing this episode, there’s an article recently in the public understanding of science that the public when looking at researchers and people who have self admitted to using things like psychedelics, that they perceive their work to be lower or less quality than people doing the same kind of work but without the self admitting piece. Katie and I are big fans of people owning their story and talking about their personal experiences with stuff as appropriate with clients. But this seems to be one area where that might actually potentially hinder some clients access to what seems to be a really great treatment.
Dr. Craig Heacock 18:35
Well, first of all, my suspicion is everybody doing research on psychedelics has done psychedelics, because, you know, research is me-search. You know, what percentage of people doing eating disorder research have had an eating disorder? I mean, 99.999, what percentage of addiction therapists anyway, so I yeah, I guess what I think I’m curious if you’ve experienced this, Curt, I know you’re a runner. I’m a runner. I have some people come to me and say, you know, you’re serious runner. That’s one of the reasons I chose you. I’ve other people say, it took me eight months to call you because I see you’re a serious runner. And I think you’re gonna shame me. You’re gonna make you’re gonna think I’m lame and lazy and you’re not, you’re already not gonna like me. I think: Just because I’m a runner? So I guess when I saw that article that you sent me, I thought, well, yeah, people come up with all sorts of stories, researchers doing microdosing, or therapists who are runners or therapists who admit that eating disorder. Yeah, I mean, all those people doing psychedelic research, have done psychedelics. So maybe we should just say that, like, get over it, people. That’s why they’re doing this research.
Curt Widhalm 19:39
It’s whether or not they’re out there publicly owning the stories out of this.
Dr. Craig Heacock 19:43
Yeah, yeah. So and more and more people are talking about it. It’s really interesting, even one of my favorite podcasters Peter Attia, who’s a doc and he’s openly talked about his psilocybin experiences. And of course, Tim Ferriss has and, and Tim Ferriss talked about his MDMA experiences. People, some powerful people are openly speaking about how psychedelics have really furthered their trauma work and moved them forward in life. So I really think we’re at Malcolm Gladwell’s tipping point. You know, I remember in Colorado years ago think, Gosh, will weed ever be legal? There’s no way and all sudden, boom, not only is weed legal, it’s everywhere. And it’s, you know, high octane, THC wax and shatter, and it just happened like that, or, you know, gay marriage. Same thing, like, There’s no way that’s gonna happen, boom. And now, it’s amazing. Like I get, literally get 70 year old women coming into my office for a session like, do you think I should micro dose? How would you recommend that I take shrooms? You know, like, are you serious? I mean, this happens, or I just had an email the other day, and this woman said, Well, I’ve been in bed a year depressed, but what got me out of bed was psilocybin. And so she’s telling me her whole story about that. And what do you think about that? I said, Wow, that’s great. She said, I’m not all the way better. I need your help. But this is common now that people are coming in. These aren’t just like, you know, 20 something, you know, stoner guys, these are grandmothers and high school principals who are coming in. Hey, I had an ayahuasca journey last year, and I’m thinking about doing, you know, DMT with the underground sitter that I found, like, what do you think about that? So I think, you know, everything doesn’t change until it does.
Katie Vernoy 21:22
That leads me to the question of kind of more, this underground scene seems to be coming out into the open. And I think there are also legislation things that are following to support the ability to use these things. I mean, what, what needs to happen for this to become kind of best practice and in the mainstream, do you think?
Dr. Craig Heacock 21:47
Yeah, that’s, that’s a huge question. So well, let’s just talk about let’s be very concrete, let’s talk about psilocybin. So psilocybin from psilocybin mushrooms, very likely will get FDA approval for treatment resistant depression in the next two or three years. The phase three trials are looking really good. How’s that gonna roll? It’s, I mean, I think there’s a really good chance that in Colorado, psilocybin might be decriminalized or even legalized before it’s medicalized. You know, with marijuana in Colorado, we had medicalization, which actually was kind of nice to do that first, I think to kind of break it into full legalization. But I psilocybin is something that, again, because the tides turning so quickly, I wouldn’t be surprised if it’s decriminalized or legalized first, which would not be my preference. Because I would hate to have it used so indiscriminately that then it got locked away forever and couldn’t be used in medicine. So, there’s definitely in the psychedelic kind of community, there’s a real split between the medicalizers, at least the initial medicalizers, I would put myself in that boat like, let’s medicalize these things first, and control and control and see versus more of the libertarian: this stuff’s coming anyway, you shouldn’t be told what you can and can’t put in your body. And why should we let the medical community control these things? Let’s, let’s bring it on, full steam. So and again, probably like this happening more and more in the US, it’s going to be state by state. If you want to buy big guns, you go to Wyoming if you want big fireworks to go to Wyoming, if you want psilocybin go to Colorado.
… 23:17
(Advertisement Break)
Curt Widhalm 23:17
Even within this medical context, Katie and I being in California, where there was the the medical marijuana before things have have opened up to where things stand now. Even some of the approach to the medical stuff seems kind of like just a joke that you know, you go down to Venice Beach, you go down to Venice Beach and give a doctor 40 bucks and literally claim any ill to get medical marijuana. How does that fit within this conversation in the medical versus, you know, kind of opening things up decriminalize sort of space?
Dr. Craig Heacock 23:55
Yeah. I think… I have a lot of strong opinions on this. I did an episode on this in the first season called Can, I think it was called Can marijuana Really Be Medical. But I looked at this psychiatric idea. There’s all sorts of people that have green cards, medical cards in Colorado for depression, PTSD, but interestingly, these people are using mostly using really high potency strains of THC or just full on THC as opposed to CBD that is making things much worse.
Katie Vernoy 24:28
Yeah.
Dr. Craig Heacock 24:28
So I mean, if I were the, the dictator of Colorado, I would eliminate medical marijuana and just say: Come on, get real. This is recreational if you want to use it medically for your glaucoma or your chemotherapy nausea like do that. But in Colorado, if you have a medical card, you can get weed way way cheaper. So I know a lot of people that get their monthly ration way cheaper and then they sell the rest of it. So they use a good chunk of it. They sell it to subsidize so they basically become kind of subsidize dealers. Which is like, let’s just, let’s be honest, let’s just get rid of this ridiculous medical distinction just make it all recreational and tax it heavily like the recreational is. But I do I sometimes think I spend half of my time with patients talking about weed or sleep. Sometimes I biked home from work and I think I’m a weed and sleep doctor. You know, meaning like trying to get people to sleep better and trying to get people to not use so much high potency weed. My take on that, as you know, growing up in the 80s you know, the weed we had was like Coors Light, it was 4 or 5, 6% by way of THC. Weed now is like Everclear 35, 40, 45% THC by weight or you just buy straight up THC. And it we’re regularly seen people have psychotic breaks. If somebody told me 10 years ago, oh, you’re gonna regularly have patients like run around naked with weapons because of marijuana. Id say there’s no way but actually to be technically accurate. It’s not usually people smoking flowers, people using THC, wax and shatter. But I probably have two or three patients a month go psychotic from from THC. And can’t you have so many people come in? Oh, I’m having panic, you know, but there’s, you know, they’re using $200 of THC a week. Like oh it helps me it is not helping you. It just is no. So we do, in Colorado, we’re doing a lot of damage control with people we’re using these really high potency strains. And what I tell people is like, look, please, like you’re using Everclear just drink beer meaning don’t, don’t vape wax, don’t smoke, shatter, like just smoke like a regular bud have lower potency THC. And that will probably be okay. But it’s a constant fight with people. And again, part of it, I think is people like, oh, it’s medical. It’s treating my illness. That’s not helpful. That is frustrating. So I think it could help people in general, if we could just get rid of this idea like, hey, it’s recreational. It’s a coping strategy, fine. But this whole idea like, Oh, it’s my medical this is, this is my treatment at least psychiatrically I think that’s largely bogus.
Katie Vernoy 27:09
Well, that’s very validating to me, because that’s been kind of my opinion, as well. So yeah. It’s recreational, it’s fine. Sometimes it’s good. But it’s like, I think the issue here is kind of what should be regulated and what and medicalized and formulated and what could be recreational? And I think, for me, because I hear about people kind of creating their own micro dosing or identifying, you know, what, how much THC they want to have, or those kinds of things. And it’s, to me, it feels like, because of how hidden and illegal and all of that stuff that most of these substances have been, it feels like people as as the door is opening, people are like, Oh my gosh, and it’s like, candy jars in the waiting room. It’s like, how best if someone is thinking, I need something different. And I’m thinking more from a client perspective, or therapist helping their clients make some of these choices or navigate some of these, these issues around whether they’re actually recreationally using something or getting medicine. But how should people consider how they go about some of this stuff? Because to me, I’m, I’m hearing people saying like, why micro dosing, and it’s like, Well, under a physician’s care, or you just only smoking little, or taking a little like…
Dr. Craig Heacock 28:27
When you say micro dosing you mean marijuana? Is that what you’re referring to?
Katie Vernoy 28:30
No, I’m just I’m speaking broadly. I mean, I think people are like I’m micro dosing X, you know, like, whatever it is, but I think these things need to be under medical care, you’d like a physician’s care is what I’m hearing, in order for it to be safe and effective, versus there’s some stuff that’s recreational that people should just say, this is recreational and it’s not my medicine.
Dr. Craig Heacock 28:52
Again, I think it’s very substance dependent. Microdose excels and seems very, very, very safe. But I know people have a number of patients that even at the tiniest bit of THC can flip them into mania or psychosis, tiny amounts. So yeah, in general, we think of marijuana as being pretty safe. But for some people, THC is completely destabilizing. We don’t see that with psilocybin. And then you can’t really microdose MDMA because it won’t do anything. You need a certain kind of escape velocity. I think the same is true with ketamine. Well, people do microdose ketamine, but then you get into a whole other series of problems. But I think it’s good that we’re talking about these things. And I love that people are asking me. Part of me making Back from the Abyss we talk about psychedelics a lot. So I think that gives people permission. If they look on my website, they say, Oh, this is someone we could, I could probably bring this up and way better to talk about it. But what people don’t really talk about is their marijuana use. And if I get one message to therapists who are listening, you all should take four or five minutes every session and find out more about your clients sleep and their substance use because I have a lot of people come to me, who’ve been seeing therapists a long time and they, they miss the person’s using tons of weed and high concentration THC. And as I said, I often think I’m sleep and weed doctor because I’m just constantly realizing that those two factors like if you can get a good night’s sleep and not abused substances, you’re halfway there. You might, you might be three fourths of the way there.
Curt Widhalm 30:20
Your Podcast Back from the Abyss talks about emerging from the deep darkness of the human condition. Can you tell us a little bit more about what attracted you to telling the stories?
Dr. Craig Heacock 30:30
A few factors. One is in 2012, I went through my own really dark place with addiction. I’d had at that point, late [unintelligible] five suicides. I had two shortly thereafter. And then I had my first two patients murdered. And I just, I just started melting down and I, you know, I was 40 years old and thinking, I can’t do this anymore. This is too hard. This is too, it’s too sad. It’s too brutal. And then, in the last nine years, I’ve really been able to find a way to do this and not have it drag me down so much. But one of the things I really found this is making the podcast is it reminds me that people get better, that people come out of the breaks. A part of it’s for me, part of it is my self care. Part of it is my passion projects. Another part of it is episode one Elizabeth, which is a really, really powerful episode. But she’s been my patient for years. And she had been saying I want to tell my story, I want to share that you can come back from such horrific suicidality. And she was in the ICU on a ventilator after her most recent attempt and, and her story was so inspirational. And I was, as it kind of came together. Like, I want to put something out there, I thought of her. I thought of me wanting to put some hope out there. And I thought, yeah, I want to help people tell their stories. So we can spread the word that you can come out of a really dark place. And that even if it takes a long time and a brutal slog, and that it’s okay that you go back because pretty much everyone I’ve asked to be on it has said, Well, I still really go to dark places. And so that’s good. Yeah, we’re not looking for the homerun bases loaded, done, sit down, and we’re looking for the hard earned wisdom. And then when the darkness comes back, what do you do? So it’s helped me a lot. And just earlier today, before I talked to you guys, on the last episode of the podcast, I said, Hey, I want to get to know some of you. You guys want to have a video chat and meet me? So the last few days, I’ve been doing these video chats with people all over the world. It’s so fun, it’s the best thing I’ve had. So it’s not such a good pandemic thing, because I’ve just, we feel so isolated. And yeah, it’s been really cool to connect with these people that are being moved by the stories, because they definitely moved me. And it’s been, I think, almost uniformly really therapeutic for the people telling their stories because I tell them like look, choose a pseudonym, if you want to tell the story that you need to tell, I want this to be your hero’s journey. I want, you know, everybody, before I publish it, I send it to them, and they can have anything cut that they want. And almost nobody ever wants anything cut. So I really want them to feel good about the other journey. And that’s been one of the coolest things when I send the final cut. And they call me Oh, I love it. Even though they’re talking about brutal, I mean, a lot of them are. I mean, some of them are just really hard stuff. I guess you know, when we create things that help other people and helps us it’s helped me a lot.
Katie Vernoy 33:25
We will link to that in our show notes. But where else can people find you and learn more about what you’re doing?
Dr. Craig Heacock 33:31
So you can link to my podcast or learn more about me at Craig Heacock. C-R-A-I-G-H-E-A-C-O-C-K md.com. Back from the Aby is on all the podcast apps. And yeah, I want to thank you too, so much for having me on. This is really fun.
Curt Widhalm 33:50
And you can find our show notes at mtgpodcast.com. And while you’re there, you can check out all the projects that Katie and I are working on. Come and follow us on our social media and strain our therapist group on Facebook, the Modern Therapists group, and until next time, I’m Curt Widhalm with Katie Vernoy and Dr. Craig Heacock.
… 34:09
(Advertisement Break)
Announcer 34:10
Thank you for listening to the modern therapists Survival Guide. Learn more about who we are and what we do at mtsgpodcast.com. You can also join us on Facebook and Twitter. And please don’t forget to subscribe so you don’t miss any of our episodes.






SPEAK YOUR MIND