Choosing Yourself as a Therapist: Strategies to address burnout, compassion fatigue and vicarious trauma – An Interview with Laura Reagan, LCSW-C
Curt and Katie interview Laura Reagan, LCSW-C, of the Trauma Therapist Network. We engage in real talk about burnout and compassion fatigue. We look at why therapists are especially susceptible to burnout, what therapists can do to take care of themselves, and what systems we can set up to try to avoid burnout and compassion fatigue. Laura also shared some ideas for group practice owners who want to support their clinicians.
Click here to scroll to the podcast transcript.Transcript
An Interview with Laura Reagan, LCSW-C, Trauma Therapist Network
 Laura Reagan, LCSW-C is an integrative trauma therapist who owns a group psychotherapy practice in the greater Baltimore area. Laura also hosts Therapy Chat and Trauma Chat Podcasts, and she founded Trauma Therapist Network in 2021. Laura trains trauma therapists around the world in using bottom-up therapy methods and accessing their highest selves while doing meaningful psychotherapy work for sustainable careers.
Laura Reagan, LCSW-C is an integrative trauma therapist who owns a group psychotherapy practice in the greater Baltimore area. Laura also hosts Therapy Chat and Trauma Chat Podcasts, and she founded Trauma Therapist Network in 2021. Laura trains trauma therapists around the world in using bottom-up therapy methods and accessing their highest selves while doing meaningful psychotherapy work for sustainable careers.
In this podcast episode, we take a deeper look at therapist burnout work
We’ve spoken many times about burnout and compassion fatigue. We decided to revisit this important topic with our friend, Laura Reagan.
What do therapists need to know about “burnout” and “compassion fatigue?”
“My clients won’t be okay if I take a break….if I rest, if I cancel, if I take a sick day, my clients won’t…be able to survive without me. And while it is important for people to be able to count on us showing up reliably and consistently…it doesn’t build trust when clients see us not practicing what we preach, or not taking care of ourselves the way we need to.” – Laura Reagan, LCSW-C
- Burnout isn’t necessarily us not wanting to work, but feeling that the world will fall apart if we aren’t there for our clients
- Not paying attention and ending up losing our clients’ trust
- You forget you have agency
Why are therapists at particular risk for burnout?
“When I have gotten to burnout, it’s the feeling for me of everything I’m doing is like a drop of water in the ocean, it’s never going to be enough. The problem is too huge. It’s immovable. I’m just one person. And this feels devastating, because I really want this problem to be better. You know, I want a world that’s loving and just.” – Laura Reagan, LCSW-C
- Our stuff coming up and not being there for ourselves
- Not metabolizing our own trauma triggers
- Getting dissociated and numb due to our compassion fatigue and moral injury
- There are different levels of risk based on developmental stages
What can therapists do to take care of themselves?
- Identify whether there is space for experiencing emotions as well as being present for clients
- Step away when needed, even when that could mean stopping see clients
- Exploring other options to take care of yourself financially
- Learning to choose yourself
What can therapists do to prevent deep burnout and compassion fatigue?
“I think it’s more than just putting yourself into spaces with other people. But really paying attention to what you need from the relationships and how it feels when you’re getting it, and how it feels when you’re not getting it.” – Laura Reagan, LCSW-C
- Being in tune with yourself and your body
- Paying attention to your responses to a client session, day, week
- Understanding what is happening inside yourself to identify what you need to be well
- Making sure to move in between sessions to recalibrate your nervous system
- Being in community while also working to stay in connection with yourself
- Specific suggestions for group practice owners
Resources for Modern Therapists mentioned in this Podcast Episode:
We’ve pulled together resources mentioned in this episode and put together some handy-dandy links. Please note that some of the links below may be affiliate links, so if you purchase after clicking below, we may get a little bit of cash in our pockets. We thank you in advance!
Instagram: @therapychatpod; @batraumahealing; @traumachatpod
Facebook: @therapychatpod; @lauralcswc; @traumatherapyconsulting
Our Linktree: https://linktr.ee/therapyreimagined
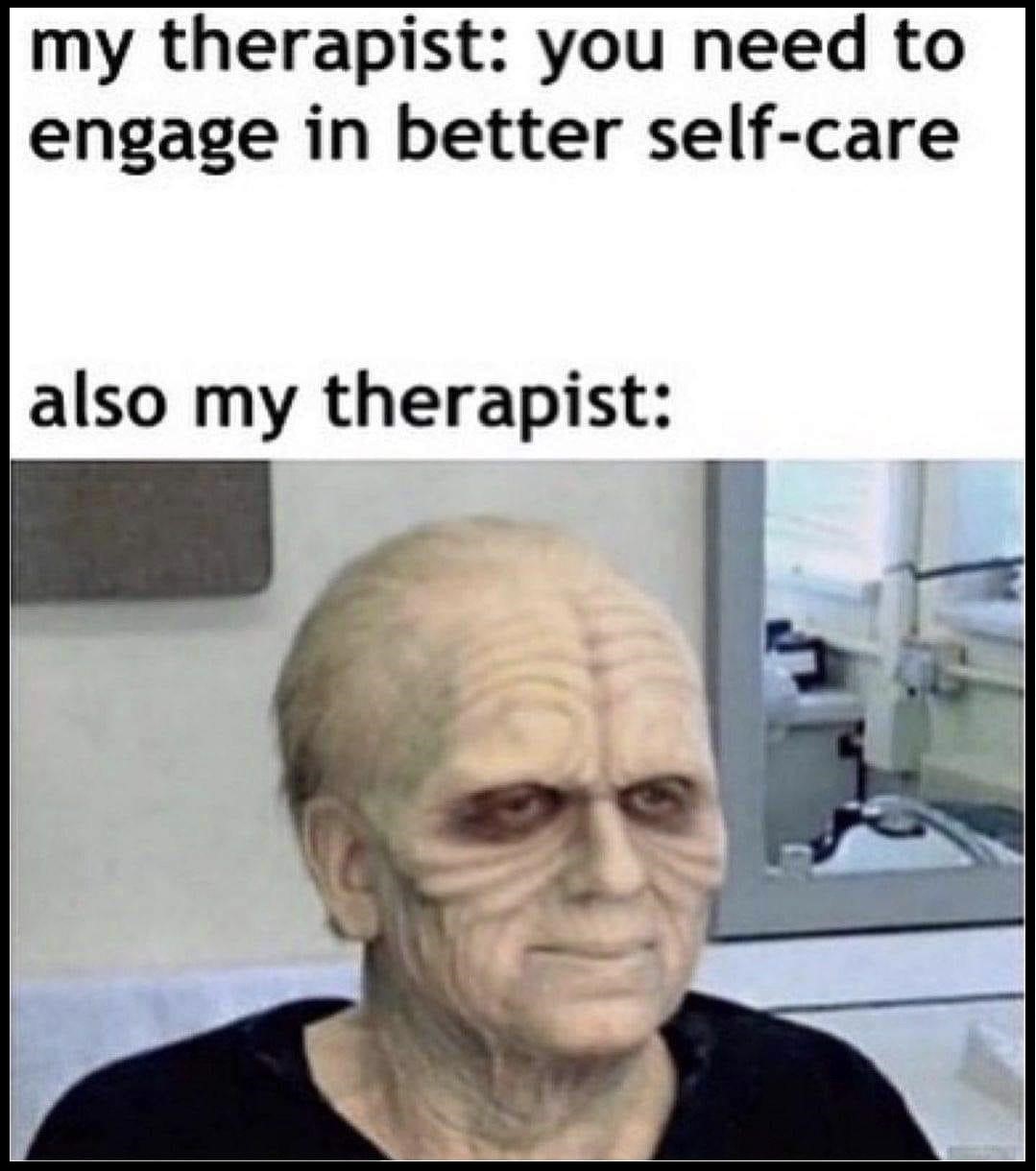
Palpatine Meme mentioned in the episode:
Relevant Episodes of MTSG Podcast:
Laura’s other 2 episodes
Are You Even Trauma-Informed? An Interview with Laura Reagan, LCSW-C
Managing Vicarious Trauma: An Interview with Laura Reagan, LCSW-C
—
Who we are:
 Curt Widhalm, LMFT
Curt Widhalm, LMFT
Curt Widhalm is in private practice in the Los Angeles area. He is the cofounder of the Therapy Reimagined conference, an Adjunct Professor at Pepperdine University and CSUN, a former Subject Matter Expert for the California Board of Behavioral Sciences, former CFO of the California Association of Marriage and Family Therapists, and a loving husband and father. He is 1/2 great person, 1/2 provocateur, and 1/2 geek, in that order. He dabbles in the dark art of making “dad jokes” and usually has a half-empty cup of coffee somewhere nearby. Learn more at: http://www.curtwidhalm.com
 Katie Vernoy, LMFT
Katie Vernoy, LMFT
Katie Vernoy is a Licensed Marriage and Family Therapist, coach, and consultant supporting leaders, visionaries, executives, and helping professionals to create sustainable careers. Katie, with Curt, has developed workshops and a conference, Therapy Reimagined, to support therapists navigating through the modern challenges of this profession. Katie is also a former President of the California Association of Marriage and Family Therapists. In her spare time, Katie is secretly siphoning off Curt’s youthful energy, so that she can take over the world. Learn more at: http://www.katievernoy.com
A Quick Note:
Our opinions are our own. We are only speaking for ourselves – except when we speak for each other, or over each other. We’re working on it.
Our guests are also only speaking for themselves and have their own opinions. We aren’t trying to take their voice, and no one speaks for us either. Mostly because they don’t want to, but hey.
Stay in Touch with Curt, Katie, and the whole Therapy Reimagined #TherapyMovement:
Consultation services with Curt Widhalm or Katie Vernoy:
Connect with the Modern Therapist Community:
Our Facebook Group – The Modern Therapists Group
Modern Therapist’s Survival Guide Creative Credits:
Voice Over by DW McCann https://www.facebook.com/McCannDW/
Music by Crystal Grooms Mangano https://groomsymusic.com/
Transcript for this episode of the Modern Therapist’s Survival Guide podcast (Autogenerated):
Transcripts do not include advertisements just a reference to the advertising break (as such timing does not account for advertisements).
… 0:00
(Opening Advertisement)
Announcer 0:00
You’re listening to the Modern Therapist’s Survival Guide where therapists live, breathe, and practice as human beings. To support you as a whole person and a therapist, here are your hosts, Curt Widhalm, and Katie Vernoy.
Curt Widhalm 0:15
Welcome back modern therapists, this is the Modern Therapist’s Survival Guide. I’m Curt Widhalm, with Katie Vernoy. And this is the podcast for therapists about the things that we do in our work, the ways that our work impacts us, and joining our very exclusive club of guests who’ve been here three times or more, we are joined by Laura Reagan, LCSW, trauma therapy podcast… LCSW-C, I’m being corrected. And thank you for joining us, again, talking to us today about compassion fatigue, and you just work in a lot of really deep work in kinds of things. So thank you for coming and sharing your experiences in dealing with this kind of stuff.
Laura Reagan 0:58
Thank you for inviting me back. It’s so fun to be with you both.
Katie Vernoy 1:03
As you know, the first question we always ask is, who are you? And what are you putting out into the world?
Laura Reagan 1:08
I’m Laura. Who I am is I’m an integrative trauma therapist, I practice somatically and use a lot of bottom up methods in my work. And I’m located in the state of Maryland, in the United States. And what I’m putting out into the world, oooh I hope it’s something meaningful and connecting because that’s what I feel is so much needed right now that, you know, to kind of like, reconnect with ourselves, reconnect with each other, and with presence. So I do that by podcasting, I have two podcasts, Therapy Chat and Trauma Chat. And I have Trauma Therapists Network, which is a website resource. And then I also own a group practice in Maryland, not seeing clients currently in my therapy practice, but I also offer coaching, so I do a lot of things, but not nearly as much as I used to.
Katie Vernoy 2:09
You’re getting better, you’re getting better.
Laura Reagan 2:11
Yes, I’m moving in the right direction.
Curt Widhalm 2:14
You talk a lot about compassion fatigue, vicarious trauma, moral injury, a lot of this kind of stuff. And I think as a field, you know, we do a really good job, from our experience point of view, talking about people entering into the field, like, you know, these are things to be aware of, you know, have these practices, so you don’t burn out. And I see a lot of early career clinicians being like, is this compassion fatigue? Is this burnout? Is that what I’m feeling? And I think, you know, talking with you and other people who really are in kind of some of this deep workspace, there’s the idea of what it is when you haven’t had it yet. And then there’s the way that you experience it when it’s actually there. And it can happen to any and all of us. I guess, maybe in getting this conversation started is what do therapists miss when they first start getting into this realm?
Laura Reagan 3:09
That’s a super great question. Because I think what we miss so often is how much we’re impacted. What I’ve experienced when burnout came knocking, is that I felt more indispensable. So while you would think that burnout would make you feel like you don’t want to work anymore, what I observe is that it makes people feel like they should be doing more and more and more, and there’s no amount of giving that could ever be enough. So what we miss is that we are suffering, and we think I won’t, my clients won’t be okay, if I take a break. You know, if I, if I rest if I cancel if I take a sick day, my clients won’t, you know, be able to survive without me. And while it is important for people to be able to count on us showing up reliably and consistently. That is an important part of what makes therapy work and what makes the therapeutic relationship trustful or builds trustworthiness. Also, it doesn’t build trust when clients see us not practicing what we preach, or not taking care of ourselves the way we need to. I don’t know if you’ve seen that meme. It was definitely going around during the pandemic where there’s a person wearing like a costume or makeup that kind of looks like the….
Curt Widhalm 4:45
The Emperor Palpatine one.
Laura Reagan 4:46
Was that what it is?
Curt Widhalm 4:49
We will include all memes discussed in this episode in our show notes at mtsgpodcast.com.
Laura Reagan 4:56
It’s like my my therapist you need to practice more self care. Also my therapists and the image is like, ah, you know, this person who’s looking like The Walking zombie. And I think that’s very real, especially now, especially now.
Katie Vernoy 5:13
You’ve talked recently about your own deep compassion fatigue, vicarious trauma, and I know more recently about some grief. Can you talk a little bit about your journey? I think it helps to really elucidate this deeper burnout. It’s not just the burnout of like, Hey, I’m not making enough money. And oh, I’m feeling exhausted. It’s this this deep, deep level, you’re able to talk about it better. So I’ll just let you do that.
Laura Reagan 5:40
Yeah, so I haven’t really defined what I’ve been going through recently as straight burnout. I think what it is, is really burnout prevention, because I’ve, I know that I was, I was on that path. And if I didn’t make some serious changes, I was going to lose myself completely and lose my ability to show up. But I think that what’s so insidious about the way that compassion fatigue, secondary traumatic stress, vicarious trauma, burnout can impact us is that what’s happening is our stuff getting activated, us basically re-experiencing, being there for someone else, and not being there for ourselves. And I think that that is a dynamic that many of us have experienced in childhood where in some way we felt needed. We wanted to feel needed, we wanted to help. And it’s like a do over of the helplessness of seeing someone suffering, like mom who was depressed or something like that. You know, your caregiver wasn’t able to meet your needs, because they were blank, exhausted, traumatized, always working, struggling to survive in some way. So we want to be the person that is there for everyone else. And when we sit there with clients and absorb their pain without having a way to process it through and let it metabolize through us, you know, we just are taking it in and holding it, and then it opens up ours, and then we’re in our own trauma activation. And then again, it can, you know, bring up this helplessness. And I think that’s what really, the compassion fatigue is, is we become numb, because we’ve begun to have this frozen helpless part of ourselves be what is most present in our lives. I mean, when you work with abuse, and childhood trauma, and you hear, not just the things like when you talked about moral injury, it’s not just the things that like accidents and things that happen that are terrible and tragic, but it’s things that people do to each other, to hurt each other. It’s just so disheartening, and when you’re hearing it over and over and over.
Katie Vernoy 8:15
Yeah.
Laura Reagan 8:15
And then when you have that in your own history, and I do, of course have many experiences of you know, being exploited, abused, mistreated, unappreciated, abandoned, betrayed, whatever, all of them. And I’m not making light of those. Those are major experiences.
Katie Vernoy 8:36
Yeah.
Laura Reagan 8:36
Major pain points. And so when I see these people who’ve been through all these things, and I’m hearing it over and over, it’s just becomes this kind of, it’s like, your world closes, and you start to be like, everything is so bad and dangerous and hopeless. And I’ve, I’ve experienced, okay, so when I have gotten to burnout, it’s the feeling for me of everything I’m doing is like a drop of water in the ocean, it’s never going to be enough. The problem is too huge. It’s immovable. I’m just one person. And this feels devastating, because I really want this problem to be better. You know, I want a world that’s loving and just, you know, and obviously, justice is a construct. But…
Katie Vernoy 8:36
Yeah.
Laura Reagan 8:38
And is there right and wrong? My Buddhist therapist says no. But so, you know, it just it wears you down and wears you down and when it’s activating those parts of you that have that same pain, it can take you out.
Curt Widhalm 9:47
How does that impact the clinical work? And after that, very in-depth description, please provide our listeners with some hope that there’s ways of rebounding back from this.
Laura Reagan 9:59
Well, I’m sitting here laughing. So yeah, there’s definitely, you know, I feel like our, our work is really joyful, because we can help. One example of a definition of trauma is that it’s too much, too fast for your nervous system to be able to process it. So whatever’s happening is too big, too painful, too scary, too much, and you can’t integrate it into your experience. So if you think about clinical work, if you have 10 clients a day, and each one is a child who’s living in an abusive home, and you’ve reported five of them to CPS, and the reports were not addressed, or, you know, the child recanted, and then nothing happened. That’s too much. That’s too much. You know, when you aren’t getting like a separation from that, it feels traumatic to you. So what has made the biggest difference for me in my life, and this is why I stopped seeing clients last July, not forever, but for now. Because both of my parents are elderly, and in poor health, and I didn’t have the space to feel my feelings and be there for my clients. So what I would do is be there for my clients. And not let myself feel my feelings. But there was, there were parts of me that were screaming, I need space to grieve and in process my fears and, and how my childhood trauma with these parents is coming up, as I anticipate losing them. And without that space, you know, I’m sitting with clients, and I’m giving them the most I have to give, and I’m giving myself nothing, which means I’m numbing myself to myself. So I think that’s what compassion fatigue is, it’s just a form of dissociation where you’ve needed to distance and distance and distance from this overwhelming pain, and so you’re numb, and then you lose your capacity to be able to connect with your empathy and compassion for the person anymore. Because you’re, you have to numb and it’s unconscious, of course.
… 12:27
(Advertisement Break)
Katie Vernoy 12:28
And I think numbing in some ways is better than the alternative when you’re in that situation, because I’ve seen folks just take more and more on and, and a lot of us, in the research I’ve done are, we’re parentified children.
Laura Reagan 12:42
Exactly.
Katie Vernoy 12:42
That was our role. And then we’re not giving anything and especially for hearing a lot of either similar stories, or just stories about how people can be pretty awful to each other and do horrible things, we can start to lose trust in humanity, it can feel like it’s hopeless. And, and we’ve got episodes on on therapist suicide, suicidal therapists, so we don’t need to go into that here. But there’s that element of the pain becoming too heavy to take that that seems like an option. And so there’s that, that element of, as therapists, we have to figure out how we’re going to take care of ourselves in these situations, and there’s systemic things as well. But but we also have a responsibility to ourselves, and it sounds like for you, that was for a period of time not seeing clients. How did you make that decision?
Laura Reagan 13:31
Well, it was not easy at all, to tell you. And my therapist was recommending, well, he wasn’t saying you should stop seeing clients. And I’m glad he didn’t say that, because I was like, afraid he was gonna say that. And I did not want to hear that. Because I don’t want to not be able to do it. You know, I don’t want anybody telling me, I can’t do it. And I certainly don’t want anybody to tell me that you’re doing harm. And I don’t want to do harm. But what my therapist kept telling me was, you need more space for your feelings, you know, you’re not having the space you need to be able to allow these feelings. So basically, I think what I was doing is kind of like, would allow them during my therapy session once a week for an hour. And then I would feel them later. But then, you know, I would try to kind of pack them back up, put them away and not deal with them. So when my mom had a stroke in February 2022, that was such a wake up call to me that I said, first of all, I don’t want to have a stroke. I don’t want to have a heart attack. And I also don’t know how much longer I’m going to have my mom. So funny that I’m going to say this but it’s like I don’t want to be taken out of being able to work because I’ve loved this work so much. But I also need to make a living. So you know I need to be able to work to survive. Unfortunately, in our capitalist world, that’s how it is. At least capitalist culture in the US. So I realized I was under so much stress that I was putting myself under, you know, as you’ve known me for a while, Katie. And you’ve seen how I keep doing more and more and more, like you were saying. So, something clicked when my mom was in the hospital, and I said, I can’t keep doing this. The responsibility of the weekly caseload like I loved my work. And so it was such a conflict. I’m like, I love this. I’m not feeling numb to my clients. I’m not. I don’t feel like I’m doing bad work. But the burden of every the thought of canceling, the thought of needing to reschedule, the thought of saying, I have to take time off, because I’m a family emergency over and over again. I was like, this is the burden that’s weighing me down of the work. So I need to, I need to tend to myself here. And I realized that I was actually choosing me, choosing me. And I think what was the most impactful thing about that was that I don’t think there’s another time that I can, that I’m aware of where I said, I don’t have to. It’s not a force thing somebody’s making me do or taking something away from me, because I can’t, I’m choosing me. And that was like, for my healing process. That was a huge, huge shift. I don’t know if I can even convey that really, but it felt it was like, Oh, wow. Oh, I don’t have to do this. I’m doing it for me. When have I ever done that?
Katie Vernoy 16:58
I think a lot of therapists don’t choose themselves most of the time. I mean, there’s there’s a lot of a lot of conversations we’ve had about that. We don’t need to belabor it, but to hear the joy. I don’t know if that’s the right word. But to hear the joy you had and saying, I finally chose myself, I finally chose me. That’s, that’s pretty amazing.
Laura Reagan 17:23
And it’s like wonder, too, because I didn’t know I wasn’t until I did it. Because I kept grappling with. Am I failing? Am I giving up? Am I not able to do this? Is he taking my he, my therapist, taking this away from me? Which he wasn’t. In no way he let me know, it was my choice. But it’s like, I’m even saying he let me. But now see, and that’s part of the trauma like enactment is that you, you know, you forget you have agency. That’s one of the things about burnout, that you know, how it sneaks up on you.
Curt Widhalm 17:58
And coming back to the thought trying to help other therapists put these things in place before they run into these problems. And is there a way to help this resonate with therapists before they get to this point. We, in all the guests that we interview, the stories that we hear from people who listen to our podcast. We hear people who hit this point, the, the ones who were, you know, the experts on compassion fatigue are the ones who hit it the hardest. Is this something where to really have this be a a resonating principle like this, is this something where somebody has to go through that experience?
Laura Reagan 18:39
I don’t think someone has to go through it. But I do think that it is a developmental process,. That there’s so much variation in how, where people are in their emotional development at the time they joined the field. But especially when people join when they’re in their 20s, which is pretty common. I think developmentally, if you you know, if you think about where you are in your emotional development in your 20s, there’s a certain level of self awareness that you can have based on where you are. And when you’re in your 30s, you know, just using age as a general metric, because we’re all at different places. But when you’re in your 30s, it might be a little different. And when you’re in your 40s, it might be a little bit different. And other relationships you have, you know, if you’re in or not in a longer term relationship, or if you’re parenting or any of those things, all of those things can activate our trauma and make us recognize things about ourselves that we may not have recognized before that opened up or what trauma history we have and when things happened. So that’s one reason that I sort of danced around that when you first asked it because I think it depends on where someone is. I don’t think there’s anything that anybody can do. Just step by step by step manualised kind of thing as you start, but generally being in tune with yourself is a major part of it. So probably being in tune with your body is a major part of it. If you notice that you feel exhausted after an eight client day, then asking yourself, at what point you know, maybe doing like, an experiment with yourself. Okay, I noticed I’m exhausted today, I noticed I’m exhausted by Friday, whatever it is, let me go back and look at this next week. When I go through my day, I’m going to notice what’s happening in my body throughout the day? Are there certain times of the day that I have more energy? Are there certain times of the day I have less energy? Are there certain client situations or client personality traits or dynamics between me and a certain client, that bring more of a feeling of fatigue or more of a feeling of anxiety or activation, or I don’t know what to do, when I’m with this client, I feel stuck, I feel lost. Those are the kinds of kinds of things that you would track to help you really observe within yourself, what happens for you throughout the day. And then, you know, I like I can’t imagine myself not working with trauma survivors, because just doesn’t seem interesting. And I don’t want to say, because because the work is so deep, and complex, that’s really, really interesting and fascinating to me. But if we were working at a really surface level, even if the person does have a trauma history, if they don’t want to work at a deeper level, it doesn’t feel interesting to me. And so is that because it’s activation inside of me, you know? Maybe, but what lights you up, and what pulls you down, and, and paying attention to what’s happening inside of yourself can help you structure your practice around what you need to be well. So it’s really like, you know, it’s all the stuff of your body, how you sleep, you know, what you eat, how much you move. I went to a training earlier this year with Dr. Arielle Schwartz, who I’m a huge, huge fan of, and she practices with somatically using a lot of polyvagal theory. And she said that our bodies need to move every 45 minutes just as our natural bodies rhythm. That’s what some studies have showed. And if you think about, of course, our sessions are usually 45 to 50 minutes. And for many of us, it goes right up to the hour. And then sometimes it’s back to back. And we might not even, especially for on virtual, we might not even get up out of our seat. So one simple thing that people can do to tend to nervous system wellness is just to make sure to move every 45 minutes or so. And just be aware that your body needs that. So for me, that’s a major shift from the idea of like, oh, I should be going to the gym, oh, I should be working out, oh, I should be exercising every day. That’s not necessarily the point of this. This is more about giving yourself, you know, one to two minutes of movement, at least every 45 minutes, just so your nervous system can recalibrate. Even if it’s like a balance posture, and yoga like, you know, just something very simple, like balancing on one leg for a minute and then the other leg and just that like allows your nervous system to re calibrate itself and come back to center. I don’t think there’s any any simple thing that people can do. It’s really about getting to know yourself.
… 24:05
(Advertisement Break)
Katie Vernoy 24:06
You’re talking about emotional development, you’re talking about giving yourself permission to take care of yourself. I think these are all things that therapists see as positive but don’t necessarily give themselves permission to do. And for me, I think when I look at the the times when I’ve had deep compassion fatigue or burnout or those types of things, it’s often been that I felt so very isolated and alone. And I know you talk about healing and connecting within community. And to me that that feels really important. And that was the thing when I went from Community Mental Health to private practice that I felt very deeply it was I had all these people I could walk down the hall and talk to and now I’m by myself. How does community fit into this?
Laura Reagan 24:51
Yes, definitely. I think connection is so its connection with yourself and connection with other people. Because you know we can be spending time and community but still only focusing on everyone else and not ourselves.
Katie Vernoy 24:51
Yeah.
Laura Reagan 24:58
You know? It’s funny that you said that about agency to private practice, people often say how isolating private practice is, and it can be, but I was it isolated in agency work, too. And for me, it was like, I might have had some people at work that I liked. But I didn’t really feel like they got me. I was isolated, because I was isolated. They were there. But I didn’t really want to talk to them. Or if I did, you know, it wasn’t really meeting what I needed from it. So I wasn’t like giving it that potential to be what I needed it to be. So I think it’s connection with yourself. It’s being in community, but it’s, you know, even who we spend time with, and how we feel when we’re with those people. A lot of the people that I have surrounded myself with in my life, kind of remind me of my older sister, who was basically like my substitute mom. So I have a lot of friends who are the same age as my sister, and kind of have similar personality characteristics to hers. But then my sister is my, you know, not good enough mom, because she was a child, too.
Katie Vernoy 26:27
Yeah.
Laura Reagan 26:28
So. So if all my friends are not good enough moms, then I’m not really getting what I need, you know, psychodynamically, they’re not bad moms. But you know, if that’s what I’m projecting…
Katie Vernoy 26:41
Yeah.
Laura Reagan 26:42
If I’m projecting, oh, I want something from a friendship with you, but I receive it in the same way that I do my disrupted attachment from childhood, then I’m still not gonna get anything out of it. So I think it’s more than just putting yourself into spaces with other people. But really paying attention to what you need from the relationships and how it feels when you’re getting it, and how it feels when you’re not getting it. Because what we tend to do, again, using that reenactment word, it’s like, we do it the same way we did it, because we’re trying to get that do over from childhood trauma, but we’re still going the expression going to the butcher to get flowers or whatever. Like, we’re still approaching it with the same energy of I try to get my needs met by somebody who’s not going to meet my needs. So if we can go into community in a way of being open, with an open heart and knowing what we need, not expecting the community to read our minds or know what, you know, know what we should want or Okay, here I am now. Do it for me, you know?
Katie Vernoy 28:02
Yeah.
Laura Reagan 28:02
So I think it’s, it’s like finding where your the spaces are that you feel you’re able to be in your highest self.
Curt Widhalm 28:12
As a group practice owner, do you put things into place, even before your clinicians run into these kinds of things?
Laura Reagan 28:21
That’s a good question. I would like to make everyone think that I’m like the best group practice owner around but I know my staff would be like….
Curt Widhalm 28:29
There’s no reason to dispel that myth.
Laura Reagan 28:33
Oh, yes. Well, let me tell you all the things I do. Well, now what I tried to do is in my I tried to model for my team, being my authentic self, being imperfect, having compassion for myself, being self aware, being attuned to myself, paying attention to counter transference and transference, allowing vulnerability. I think that’s the biggest thing is I try to model with the way I have my practice setup, I insist on paying a living wage, which means a pretty high wage. I insist on a lower caseload. That’s why we don’t accept insurance. I try to model healthy boundaries around work, overwork, you know, I’m not saying a few things now, but yeah, I just tried to teach them that it’s okay to acknowledge that you have trauma too. We all do. You know, we we aren’t above our clients. We’re not power over. We’re walking alongside. We know some things to help but we don’t have all the answers and we don’t have to have all the answers and we don’t, we don’t rescue we don’t you know, want people to feel dependent on us. This is something I saw someone say the other day, it’s not just what you say, but it’s how you are. And that’s what I try to model. Wellness, authenticity, self compassion, if they’re sick, I don’t want them to come to work. If they need to take a month off because they’re having a personal crisis, I want them to take a month off. Yeah, business-wise, I need them to be seeing clients, but I also don’t need them to be unable to see clients and going and seeing clients anyway. I mean, that’s harming clients, obviously.
Curt Widhalm 30:32
Where can people find out more about you and all of the work that you’re doing?
Laura Reagan 30:39
Everything I’m doing is on traumatherapistsnetwork.com; the podcast and there’s a membership community for therapists which is a beautiful community for people to join, come as they are, but but you know it’s for you. And you have something to offer to everyone and you can receive too nobody’s here just to give.
Katie Vernoy 31:02
And I’m actually a member of the trauma therapists community and I’ve been able to attend a couple of meetings and then also, there’s some great trainings in the background that you can look at as well. But I have used one of the things of a so I’ve got a this is a impromptu testimonial here, Laura, but you were I think you did a kind of get up and kind of do that movement and how to kind of shake off in between sessions and I’ve definitely used that in it is that moving every 45 minutes or so that’s helped me feel a little bit more grounded and in my body where I think I just get so caught up and even if I’m not virtual, I might just be sitting in my seat trying to get notes done in between sessions or doing things and it can get to a place where I just forget that I’m even that I even have a body and so it was so helpful and I think the community itself just feels really caring and wonderful. So thank you for creating it and I hope folks will take a look at I think right now we’re you’re on waitlist status, but you’ll be opening up again in the fall so that’s awesome.
Laura Reagan 32:07
Thanks for saying that, Katie. That means so much to me. And yeah, it’s very experiential. That’s what we want people to get. It’s not just we’re not there just talking about trauma. We’re experiencing self care and movement and you know, being together. Present.
Curt Widhalm 32:28
We will include links to all of Laura’s stuff in our show notes over at mtsgpodcast.com. And join us in our Facebook group, the Modern Therapists group and let us know what you think of the episodes work we’re doing and connect with other modern therapists follow us on our social media. And until next time, I’m Curt Widhalm, with Katie Vernoy And Laura Reagan.
… 32:50
(Advertisement Break)
Announcer 32:51
Thank you for listening to the Modern Therapist’s Survival Guide. Learn more about who we are and what we do at mtsgpodcast.com. You can also join us on Facebook and Twitter. And please don’t forget to subscribe so you don’t miss any of our episodes.




SPEAK YOUR MIND