
What Therapists Need to Know About Menopause and Perimenopause: An interview with Dr. Sharon Malone, MD
Curt and Katie interview Dr. Sharon Malone, MD, author of Grown Woman Talk, about menopause and perimenopause. We explore the mental health impacts as well as the differential diagnosis when assessing a woman over 40 who might be experiencing this phase of life. We also talk about what good treatment can look like, including discussing the debate about hormone therapies.
Click here to scroll to the podcast transcript.Transcript
An Interview with Dr. Sharon Malone, author of Grown Woman Talk
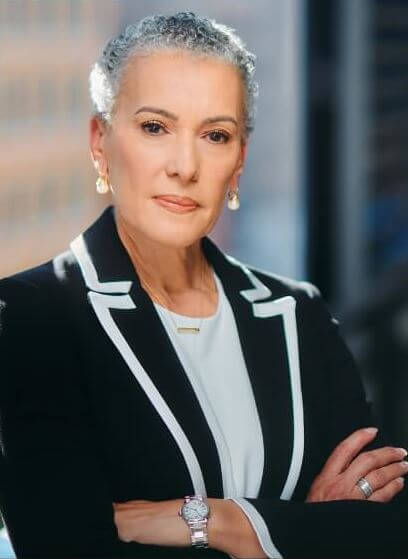 Dr. Sharon Malone is a nationally known expert in women’s health and the author of Grown Woman Talk. She is the Chief Medical Advisor at Alloy Women’s Health, a telehealth company that focuses on women over 40. Before joining Alloy, Dr. Malone was a partner at one of the oldest and most successful OB/GYN medical practices in Washington, D.C. She is board-certified by the American College of Obstetricians and Gynecologists and certified by the North American Menopause Society as a Certified National Menopause Practitioner. Throughout her professional career, she has been active in advocating for reproductive rights, reducing teen pregnancy, and eliminating health care disparities.
Dr. Sharon Malone is a nationally known expert in women’s health and the author of Grown Woman Talk. She is the Chief Medical Advisor at Alloy Women’s Health, a telehealth company that focuses on women over 40. Before joining Alloy, Dr. Malone was a partner at one of the oldest and most successful OB/GYN medical practices in Washington, D.C. She is board-certified by the American College of Obstetricians and Gynecologists and certified by the North American Menopause Society as a Certified National Menopause Practitioner. Throughout her professional career, she has been active in advocating for reproductive rights, reducing teen pregnancy, and eliminating health care disparities.
Dr. Malone is the youngest of eight children. During World War II, her parents, both of whom were raised in the rural south, moved to Mobile, Alabama, during the migration from farms to cities. She has seen health care from both sides– as a physician and a child of parents who negotiated health care for themselves and their families in the Jim Crow South. Despite living next door to two hospitals, preventative health care was never a part of her family’s life. As a result, Dr. Malone’s mother would lose her life to colon cancer, diagnosed too late for treatment. This searing life experience has informed how Dr. Malone has chosen to practice medicine and brought focus to the healthcare issues she has chosen to pursue.
In addition to her interest in women’s health, Dr. Malone is an avid reader, an amateur genealogist, and a lover of music. She is married to former U.S. Attorney General Eric Holder Jr. and lives in Washington, D.C. They are the parents of Maya, Brooke, and Eric III.
In this podcast episode, we talk about mental health impacts of (peri)menopause
After Katie was diagnosed with perimenopause, she began looking for sources of information on this seldom-talked-about phase of women’s lives. She found Dr. Sharon Malone’s work and was so excited that she agreed to come on to talk about menopause and perimenopause as well as her new book, Grown Woman Talk!
What is perimenopause and menopause?
“Perimenopause, and menopause are life stages…They’re not events. It’s not like you’re gonna get over it and then we’re on to the next thing.” – Dr. Sharon Malone, MD
- Life stages for women in midlife and beyond
- Hormonal shifts (not just dropping, but inconsistent through
- Remodeling of the brain
- Perimenopause is not short, it can be up to a decade
- Too often women think they can power through, but it can and should be treated
What are the psychological impacts of perimenopause and menopause?
“Perimenopause couldn’t happen at a worse time in women’s lives…There’s a lot going on…careers…children…elderly parents…So, all of life sort of comes in at this point. And it’s…the perfect storm for a lot of mental health issues that come up.” –Dr. Sharon Malone, MD
- Feeling different or more emotional due to hormonal shifts during up to a decade prior to menopause (when hormones drop)
- During perimenopause there is an uptick in depression, anxiety, sleeplessness, late onset ADHD, rage, brain fog
- Perimenopausal mood and psychological changes may be better treated by hormones than by typical psychotropics
- The differential diagnosis should start with ruling out perimenopause for any woman 40+
What does good perimenopause treatment look like?
- The most effective treatment of perimenopausal symptoms is estrogen or menopause hormone treatment
- Too often, women get individual symptoms treated by individual specialists rather than a more global impact of hormone imbalances
- Hormone treatments can potentiate antidepressant (synergistic effect) for mood concerns
- We also address the concerns related to hormone treatment (the study was misrepresented)
- Women should be armed with the questions to ask and collaborate and agree on treatment with their doctors
Resources for Modern Therapists mentioned in this Podcast Episode:
We’ve pulled together resources mentioned in this episode and put together some handy-dandy links. Please note that some of the links below may be affiliate links, so if you purchase after clicking below, we may get a little bit of cash in our pockets. We thank you in advance!
Dr. Sharon Malone’s new book: Grown Woman Talk
Dr. Lisa Musconi’s book – The Menopause Brain
Women’s Health Initiative Study
Women’s Health Initiative website
Relevant Episodes of MTSG Podcast:
Navigating Pregnancy as a Therapist, An Interview with Emily Sanders, LMFT
Infertility and Pregnancy Loss, An Interview with Tracy Gilmour-Nimoy, LMFT
Is BPD a Genuine Diagnosis or a Dismissive Label?
Oklahoma Bureaucrats Want Your Mental Health Records
Sex Therapy with Perfectionists: An Interview with Dr. Tom Murray
Who we are:
 Curt Widhalm, LMFT
Curt Widhalm, LMFT
Curt Widhalm is in private practice in the Los Angeles area. He is the cofounder of the Therapy Reimagined conference, an Adjunct Professor at Pepperdine University and CSUN, a former Subject Matter Expert for the California Board of Behavioral Sciences, former CFO of the California Association of Marriage and Family Therapists, and a loving husband and father. He is 1/2 great person, 1/2 provocateur, and 1/2 geek, in that order. He dabbles in the dark art of making “dad jokes” and usually has a half-empty cup of coffee somewhere nearby. Learn more at: http://www.curtwidhalm.com
 Katie Vernoy, LMFT
Katie Vernoy, LMFT
Katie Vernoy is a Licensed Marriage and Family Therapist, coach, and consultant supporting leaders, visionaries, executives, and helping professionals to create sustainable careers. Katie, with Curt, has developed workshops and a conference, Therapy Reimagined, to support therapists navigating through the modern challenges of this profession. Katie is also a former President of the California Association of Marriage and Family Therapists. In her spare time, Katie is secretly siphoning off Curt’s youthful energy, so that she can take over the world. Learn more at: http://www.katievernoy.com
A Quick Note:
Our opinions are our own. We are only speaking for ourselves – except when we speak for each other, or over each other. We’re working on it.
Our guests are also only speaking for themselves and have their own opinions. We aren’t trying to take their voice, and no one speaks for us either. Mostly because they don’t want to, but hey.
Stay in Touch with Curt, Katie, and the whole Therapy Reimagined #TherapyMovement:
Consultation services with Curt Widhalm or Katie Vernoy:
Connect with the Modern Therapist Community:
Our Facebook Group – The Modern Therapists Group
Modern Therapist’s Survival Guide Creative Credits:
Voice Over by DW McCann https://www.facebook.com/McCannDW/
Music by Crystal Grooms Mangano https://groomsymusic.com/
Transcript for this episode of the Modern Therapist’s Survival Guide podcast (Autogenerated):
Transcripts do not include advertisements just a reference to the advertising break (as such timing does not account for advertisements).
… 0:00
(Opening Advertisement)
Announcer 0:00
You’re listening to the Modern Therapist’s Survival Guide where therapists live, breathe and practice as human beings. To support you as a whole person and a therapist, here are your hosts, Curt Widhalm and Katie Vernoy.
Curt Widhalm 0:15
Welcome back modern therapists, this is the Modern therapist’s Survival Guide. I’m Curt Widhalm, with Katie Vernoy. And this is the podcast for therapists about the things that go on in our field, venturing into parts of our education that we barely touch on or don’t touch on whatsoever. And in all of the years that we’ve been podcasting, and all of the years of my experience, as we were preparing for today’s episode, I was like, this is something that I don’t think was covered in any of my formal education. And we are so lucky to have Dr. Sharon Malone to come in and share all of her wonderful knowledge around the ways that menopause/perimenopause, show up in our works, the things that we should understand as clinicians on how this affects our clients. And we’re just super excited to have you. Thank you so much for joining us.
Dr. Sharon Malone 1:10
Thank you for having me.
Katie Vernoy 1:12
I am so excited. I’ve been listening to some of the podcast interviews you’ve done and interviews you’ve done on TV and just really excited to learn this information. As I mentioned, before we hit record, I am officially perimenopausal. So some of this is very self serving, and definitely something where I’m really excited to learn. Because when I started going through this myself a couple years ago, I realized there was nothing that was being talked about. There was I you know, I would try to ask people in my life and they didn’t know or didn’t remember. And so this is something that you are focusing your energy on. So, I’m going to turn this over to you with a question that we asked all of our guests, who are you and what are you putting out into the world?
Dr. Sharon Malone 1:53
Yes, as I said, thank you for having me. This is my favorite topic, by the way. And for those of you who don’t know me, my name is Dr. Sharon Malone. I am an OB/GYN board certified and I’m also a national menopause practitioner. And what that means is that for probably the second half of my career, in addition to my other gynecology duties, I spent a lot of time talking to women in perimenopause and menopause. And it also means that I’ve had, you know, special training and you know, actually been certified in this as a sort of a sub area of gynecology. But let me tell you why it’s so important is because, you know, women in midlife have really been sort of left out there to their own devices. And I think that, you know, as OB/GYNs we have been a little bit, I would say, we’re a little bit complicit in that because we do a lot of stuff as OB/GYNs and I think, I don’t think that there’s another field in medicine that does as many things over as many different age ranges as OB/GYNs do. We are on any given day, a primary care doctor, you are a therapist, you are, you know, providing counseling for contraception, you’re getting women successfully through pregnancy. And by the time we get to midlife after we’ve dealt with some of the other gynecologic issues, where you know, everyone feels like, Okay, we’re done with that. And let me just say perimenopause, and menopause are life stages. It, they’re not events. It’s not like you’re gonna get over it. And then we’re on to the next thing. And I think that the more women know, going into this phase of life, the better prepared you are. And I tell you, there wouldn’t be no other phase. Imagine if you entered puberty with as little information as women enter perimenopause and menopause. You would think that that was really something wrong with you. Because there are not just the physical changes, there are psychological changes that happen as well. And were ill prepared for them. So, what I’m putting out in the world, I am trying to get women educated such that they know what to expect when they get to this point of life. I want them to also know what their options are such that when they interact with their medical providers, or with their therapists, they have at least the thought in mind that maybe this is not something that’s isolated. It is just all part of that continuum, that we women will call the rest of our lives.
Curt Widhalm 4:26
What is it that you think that mental health providers should know about some of the psychological effects that you’re talking about when it comes to menopause?
Dr. Sharon Malone 4:35
Absolutely, the one thing that I think every mental health provider should know is that perimenopause, in addition to the myriad of physical symptoms that women have, you know, estrogen, which is the primary driver of a lot of the symptoms that show up in perimenopause. And perimenopause, let me just explain to you: those, those are the years leading up to menopause. Which means just having Had your last period. And that average age is 51. So anywhere from a decade prior to having had your last menstrual period, these perimenopausal years, the hormonal shifts that are going on during that phase, they’re more tumultuous. It’s not because it’s lack of estroge. That happens after you’ve completed menopause. It is this erratic nature of hormones sometimes overshooting, sometimes undershooting that is really wreaking havoc on your, on your brain. Not just on your physical body, you know, it’s not just a reproductive hormone. And I think that’s what I want women to understand. You know, we all know in our heart of hearts, even without one day of medical training, that women where you are in your hormonal spectrum really affects what your mood is like on any given day. Women feel different the week before their period than they do after their period, you feel different in pregnancy, you know, you notice that there is an increase in postpartum depression, because again, these rapid hormonal shifts. So, what therapists should understand during this period of transition, it is a period of time where you also see an uptick in depression, anxiety, sleeplessness. I mean, all sorts of mood disorders really start to come up during that time. And what I want everyone to understand is that it’s not isolated. So the solution to how to treat a perimenopausal woman has to be crafted within the context of knowing that it is a hormonal issue, it’s not just an isolated psychological issue. So you know, a depression or anxious mood at this point, sometimes may involve treatment with hormone therapy, as opposed to an antidepressant or an anxiolytic.
Katie Vernoy 6:53
How would you recommend doing kind of a differential there as a clinician? Because I know for myself, I can only speak from my own experience, I I’ve had some of the mood shifts, I’ve had some of those things, but there’s also kind of the brain fog, there’s the the different physiological things that can be very anxiety producing. And then there’s also just the things of life and the things that may be more kind of straight ahead, depression, anxiety, you know, all of those things. So what’s the differential that you would recommend for therapists to do?
Dr. Sharon Malone 7:23
Well, you know, that’s the the one thing that it’s really not terribly difficult to tease apart. But I do have to say that perimenopause couldn’t happen at a worse time in women’s lives, you know.
Katie Vernoy 7:34
Sure.
Dr. Sharon Malone 7:35
There’s a lot going on, you know, you’ve got for most of us, you know, you’ve had you have careers, you’re just sort of hitting your stride, you know, you’ve got probably the most responsibility professionally you’ve ever had. So you’ve got work stress. You have many of us have still have young children in the home. So, you’ve got young children to deal with, you have elderly parents sometimes that you’re dealing with. So, all of life sort of comes in at this point. And it’s, it’s a really, it’s the perfect storm for a lot of mental health issues that come up. And when you add to that, this hormonal shift, you know, I think the best way that you can sort of differentiate is that it that if you have a woman who is between the ages of 40, and sometimes even early, their earlier, 30s, mid 30s. But if you’re between the ages of 40 and 50. And you have no prior history of any other, you know, you don’t have an anxiety disorder, you don’t have a pre-existing condition. And all of a sudden, this comes up, the first thing you should think about is really perimenopause and hormonal shifts. Because, you know, again, that’s the first thing and it’s the easiest thing to fix. When you fix, when you try to deal with the mental health issues, you really have to delve a little bit deeper into ask about some of the other physical manifestations of perimenopause. And if you have two or more data points that connect, then chances are you know, at least perimenopause has to be at the top of your list of your differential. And certainly people can get depression and anxiety. And there’s also another common complaint that women have is sort of late onset ADHD, you know, and that, that part of it comes in. And let me say that we are having a little bit of a moment now and I say a good one in understanding the changes, the remodeling of your brain that happens during perimenopause and Dr. Lisa Mosconi, brilliant neuroscientists at Weill Cornell has written two books and her latest one is called The Menopause Brain where she actually you know, she has pictures that will show women in pre-menopause in perimenopause and post menopause and she’s doing PET scans to see that not only, you know, for people who said, it’s all in your head, of course, it’s all in your head. But she’s got pictures to prove it, that your brain looks different in perimenopause, metabolically is different. Physically it’s changing. And it’s got to remodel and adjust to this new hormonal environment that you’re in. And so that’s where I say, you know, for age matters. You know, if someone comes to you at 65, and they come in with these new onset things, well, perhaps I wouldn’t think of a hormonal issue. But it is probably the most common and the most under diagnosed reason for why women come in with these anxiety disorders, new onset anxiety disorder, irritability, rage, brain fog. And brain fog, it’s very scary for women, because they think, Oh, my goodness, this is something is this a harbinger of things to come. And it’s not, it’s just your brain trying to get reorganized in response to the changing hormones.
Curt Widhalm 11:02
As a male in society, I recognize that this is not something that comes up in casual conversation between me and my friends. In my practice, I work particularly with teens. And so this is not a clinical part of my practice that I end up seeing a lot. But as my practice does expand, sometimes I want to be aware of any myths that might be out there about menopause, perimenopause, in case, I or any of our listeners are like, Hey, this is something that maybe we need to point to all of the wonderful things that you just shared as being factual. But what are some of the myths that are out there that we need to be aware of, too?
Dr. Sharon Malone 11:45
You know, I think the biggest myth or misconception that that women in general have is that it’s short. You know, if I just power through this for a couple of weeks, a couple of months, it’s going to be over and I will be over it. And what I’m trying to get women to understand is that even though some of the the tumult that you experienced during perimenopause will settle down. You’re never over it. It is, as I said, it’s a phase of life. And the other thing is that I would like women to know is that if you are experiencing these symptoms, get them treated. There’s no you don’t get a bonus point at the end for having suffered, you know, for months, years and and sometimes even a decade. There’s no benefit in that. So, you know, we’ve got to get rid of that Superwoman mentality, that if you know, we’re just we just power through it, we’ll be okay. There’s a tremendous price that we pay physically. And there’s a tremendous price that we pay psychologically for not addressing the issues that we have in midlife.
… 12:55
(Advertisement Break)
Katie Vernoy 12:58
What does really good menopause perimenopause treatment look like? And maybe for some of our listeners who aren’t going through it like I am, some of the even the physical manifestations that they might be able to treat.
Dr. Sharon Malone 13:09
Right. And for for those who may not know what the physical manifestations are, the most commonly associated symptom is really hot flashes. So there’s hot flashes, there’s mood swings, anxiety, depression, brain fog, there’s dry skin, there’s thinning hair, there’s dry vaginas, there’s painful sex, there’s feeling as if your something is crawling under your skin. I mean, the list goes on and on. So that combination of things of which you may have one from column A and two from column B, and sometimes you don’t stitch them together. women complain of weight gain, there is a weight gain thing that happens in perimenopause. And mostly it’s redistribution of weight that is problematic. So, even women who don’t gain weight during perimenopause will find that there’s a shift it sort of goes more to the middle, right where you don’t want it. So. So all of these things, and let me just say, if you have one, two, 10 of the symptoms, the most effective treatment for the symptoms of menopause is estrogen or menopausal hormone therapy. End of sentence. If you have those symptoms, you can try you know, a lot of times what happens for women, they will see a dermatologist because of skin problems or thinning hair, they’ll see an endocrinologist because they’re gaining weight. They may see a psychiatrist because they’re feeling depressed, and their care really gets parceled out. But no one is really looking at the big picture of saying you know what, all of these things sort of go together. And that’s why seeing someone who at least recognizes what’s going on even if you personally cannot treat it. You can at least send them to some one to say Oh, perhaps this will be this is something you should address. And here’s another interesting piece of information about treating mental health issues during perimenopause and menopause is that what we found is that even when an antidepressant or an SSRI is appropriate for treating depression, the effect of having estrogen and an SSRI or an antidepressant together; one: the estrogen potentiate the effect of the SSRI. So, even for women who are depressed if, if the estrogen isn’t working, and if you have to add an SSRI, or whatever antidepressant you’re using, that’s helpful. But the two together are not antagonistic, they’re synergistic. So that’s also some information that in some news you can use about treating mood disorders. But as I said, treating the physical symptoms does have a profound effect on mental symptoms. And what do I mean by that, if you have hot flashes, if you have night slip sweats, you’re not sleeping, you are irritable, the next day, you’ve got foggy brain the next day, people who don’t get good night’s sleep tend to increase their risk of hypertension, it increases your weight gain, because again, you don’t make good choices when you’ve had three hours of sleep the next day.
Katie Vernoy 13:10
For sure.
Dr. Sharon Malone 16:20
Increases your risk of type two diabetes, which just means that the more unwell you feel physically, is going to make you feel unwell mentally, you don’t exercise all of the things that we know to do that do help with mood. If you don’t address the physical symptoms, then you’re going to make the mood and whatever else you’re feeling worse.
Katie Vernoy 16:53
There’s been some controversy around using hormones. And I know that that’s something where my understanding of it is that there was a study that was overstated, about the risks of hormones. Can you address that?
Dr. Sharon Malone 17:06
Yes. And you know what, I can address this as being the old person in the room because I was here before I was, you know, I we I was treating menopause before the Women’s Health Initiative. And this was this famous study that came out it will be 22 years this July, 22 years ago that really fundamentally changed how we prescribed hormones, and our attitudes about hormones. And that was a study that really cemented in everyone’s minds that association between hormones and breast cancer. Well, it turns out that that’s really probably not true, and very overblown. But the point of that study, for those of you who may not know, it was a study that was it was the largest randomized, double blind placebo controlled study, which is the gold standard whenever you’re trying to prove something and its effectiveness. That study was designed not to answer the question of whether or not hormones worked. We knew that. We had had 50 years of using hormones, we knew it worked for symptoms. And we had some studies, some fairly significant observational studies before the Women’s Health Initiative that said that not only did hormone therapy treat the symptoms, but it decreased the risk of heart disease by 30 to 50%, which was huge.
Katie Vernoy 18:28
Wow.
Dr. Sharon Malone 18:28
If you could take a medication and it would decrease your risk of heart disease. Well, my goodness, every woman should be on it right? Because heart disease is the number one killer of women, then and now. So, the study was not designed to prove the effectiveness of hormones or to see whether it worked. It was designed for the sole purpose of seeing, does this observed finding of decreased risk of heart disease, can we prove it with this study? That was what it was about. Now, you might say, well, that’s laudable. But here’s the problem with the study design, and they didn’t realize it at the time, because women don’t get an uptick in heart disease until about 10 years after they’ve completed menopause. So, when you see heart, women having heart attacks and strokes is mainly happening in their 60s, not in their 50s when women are typically prescribed hormones. So they designed the study such that it would be more women who were older. The average age of the participants in those study in that study was 63. You could be anywhere from 50 to 79 and be the study. And because the study was only going to last eight years, they wanted to include women who were kind of already on the road to heart disease. And that’s why this you know, they they picked the study and because was it’s a double blind study, they couldn’t pick women who had a lot of symptoms, because if you had hot flashes, and I gave you a placebo and you still had hot flashes, you would know, oh, I’m not on the medication and vice versa view. And so that the population that they chose was not representative of who we normally prescribed hormones for. That was the fatal flaw of that study. And the problem was because the patients were so much older. And let me let me say this is we say it’s a classic case of closing the barn barn door after the horse is already out. How were you going to do a prevention study, when you’ve got someone who’s 75, entering your study. Her heart disease risk is pretty much solidified at that point, no matter what you do, hormones are no hormones. So, net result is it didn’t decrease the risk of heart disease, as they expected. But the real reason why this study was stopped was because they saw a slight increase in the risk of breast cancer. And that was the end all of the Women’s Health Initiative. And that’s what prompted the big press conference. Because if your two top lines is that it doesn’t decrease your risk of heart disease, as we thought, and it’s going to give you breast cancer, why would anybody take it? That prevailing thought has lasted for 22 years. Until finally someone says, You know what, that’s not really what the study said. How can you extrapolate the results from a much older population, much higher risk population, that you couldn’t prevent heart disease, even if you wanted to, to the population of women who were younger. And the good news is that when we look at women who started either before age 60, or within 10 years of when they’ve actually had their last menstrual period, the benefits far outweigh the risks. And it turns out that that decrease in the risk of heart disease does matter. It happens matters when you take it. So for younger women, the risks are much lower, there is no increased risk in the in breast cancer for women who start early. That’s also the good news. So but you know how it is it’s hard to unring a bell. And there is not only women who were disadvantaged during this time, there’s a generation of doctors who have grown up in this period who think the same thing. And I think the most pernicious effect is that it has affected research into hormone therapy negatively for the past 21 years, because people stopped studying, there are a lot of other questions that we have, that we need to know the answers to. But if no one looks at it, then you know, what is the effect of estrogen on Alzheimer’s? Pretty important to know. And had we had 30 years of data which we would have had by now had the study not been stopped, we’d be able to answer some of those questions. So that’s why it’s so important that research like Dr. Mosconi is doing at Weill Cornell, is important because she’s looking at it in a much shorter timeframe. You know, we don’t have 30 years now to do that, to redo that study to find out what’s going to happen. But to be able to look at a brain a not over 30 years, but to even watch a woman as she transitions. So you know, maybe 10 years, five years of what’s happening to your brain is important, because now we can see it. Now we can see it.
Curt Widhalm 23:46
You see this showing up in people of all backgrounds? Or do you see this in women of color show up differently than kind of the broader populations?
Dr. Sharon Malone 23:57
Absolutely. You know, there is probably nothing in medicine that the the disparity of race does not rear its ugly head. But not for the reasons you think. The disparity that we see in menopause is probably more due to the lived conditions of a lot of African American women. It is about those social determinants of health that black women are are experiencing. It’s not your DNA. It’s your environment for probably 95% of the things that we that black women experience. And so yes, for black women, there’s a study that was done. An observational study called the study of women across the nation, which they actually just followed a cohort of women over 25 years just to watch them as they progressed from perimenopause through menopause, just to see what do you what does it look like? And they found that for African American women, we tend to experience menopause earlier, you know, about a year earlier than white women. The symptoms which we normally associate with menopause, hot flashes, mood flash, all that list of 30 things, black women tend to have them more severely. And they last longer. So, if I tell you that period of perimenopause lasts anywhere on average from four to seven years for black women, that lasts 10 years. Now, that’s a long time to have all of these things that we know negatively affect your performance, the quality of your health, your mental health. And so yes, we have got to look at it that way. But not just from, you know, from a race perspective, but to also look at it from the perspective of black women are least likely to be aware of the fact that these things are perimenopausal, and can be treated easily. Even when they complain, and they go see their doctors, they are only half as likely to get a prescription, even when they complain about hormone therapy. And when they get the prescription, they take it home, they’re only half as likely to take it. And that’s because of so many of the negative perceptions out there about hormone therapy. So you have a population who is most at risk, who’s least likely to even complain or have, you know, to their doctor, and when they do less likely to get a prescription and less likely to take it, which again, has very severe long term health implications for women of color.
… 26:28
(Advertisement Break)
Katie Vernoy 26:31
For folks who are going to the doctor and whether, you know, we use the the kind of popular phrase medical gaslighting, or just ignorance from the doctor. How do you recommend that they approach that differently? Because I think I think for myself, as a therapist, I want to be able to first arm myself, but I also want to make sure I can talk to the women that I see, as clients and say, like, how can we approach doctors or find the right doctors?
Dr. Sharon Malone 26:58
Right? I think that, and this was really one of the reasons that I wrote my book: Grown Woman Talk was to really arm women, and to give them the information that they need such that when you walk in the door, you aren’t necessarily just asking for their opinion. You know, you’ve you’ve done your reading, you’ve done a little homework. So you know what this means. You know what, you know, you sometimes you have to tell your doctor, what’s wrong with you. You can’t wait for them to explain it to you. You’re like, I got it. I’ve read this, I give you all the as we say it give you all the receipts, such that when you walk in, you have a pretty good idea of what it is you want, you have a pretty good idea of what your options are. And then you can just discuss those. You don’t have to start from square one. Tell me about menopause or tell me about perimenopause. Or what do you think this might be? You’re there. And let me say this, this concept of going into your doctor and asking for the medications that you want or need. That’s not a new concept. I think every time you see a medication advertised on TV, they are betting on the fact that you will see this and walk into your doctor and tell your doctor that you want that medication. But why don’t we do that for for women? Why don’t we empower women or explain to them this is why this may be important for you, and may and certainly will improve the quality of your life for symptomatic women. We sort of are still living in that world of being very paternalistic when it comes to women’s care. And I have believed and I have practiced this way for the past 30 years. I think that once you give women information, and my job is not to say, here’s the information you decide, no, my job as a physician is to give you information, give you pros and cons, I will give you an opinion, because that’s what you pay for. You know, I’m not gonna say otherwise, what do you need me? I will I will help you. I’ll help you make that decision. And I will make a case. But nonetheless, unless you are doing something dangerous or completely crazy, I respect your decision. There may be women who say yeah, I get it hormones. I’ve been waiting for this answer. And there are women that no matter I could talk from now until I’m blue in the face and they say well, and I don’t want to and you know what my job is to say, Okay, I understand that. So, let’s figure out another way that we can minimize some of your, the symptoms and some of the long term health implications that you have. That’s my job. But my job is not to tell or withhold medication because I think it’s I think I wouldn’t do that. And you know, let’s just say there are a lot of aspects of women, women’s Health right now that we’re dealing with, where people are interjecting themselves into conversations about women’s health and what decisions we make about our bodies. And that’s gotta go.
Katie Vernoy 30:15
Yeah, for sure.
Curt Widhalm 30:15
You’ve been talking about this a lot. You’re very passionate about this. I’m sitting here learning about this a lot for the very first time. And it just makes sense. Like, there’s, you’re talking about, you know, the last 20 years of kind of all of the myths and everything else that’s out there, since you’ve gotten up on your pedestal and really started shouting to the masses. Are you seeing any kind of change in the field? Are you seeing a great response to this?
Dr. Sharon Malone 30:47
I’m seeing enormous response to this. And I think that women are grateful for the information. They are saying, Oh, my goodness, why didn’t I know this? Why didn’t somebody tell me this? And let me say, this is the beauty of telehealth. This is the beauty of social media, which sometimes there’s good news and bad news about how social media hits in terms of information. I say there’s a lot of data out there. But you can’t really evaluate it for its utility, because you don’t know what’s good data and what’s bad data. But if you find respected sources, that make sense. This is an opportunity for me to have the conversation that I’ve been having, literally for 21 years since this study came out. And I’ve been trying to explain to women why No, no, it didn’t really say that, or that doesn’t really apply to you. Well, I could talk one on one all day, and I couldn’t get to a fraction of the women that you know, even this conversation will get to. So yes, I think that that’s really important. I think that women are thirsty for this information. And let me say and it’s not just a you know, it’s not just women who were, oh, well, you’re poorly educated, or you’re uninformed. This is across the board. Every room that I go into, it doesn’t matter whether they’re PhDs or social workers or, you know, cafeteria workers, the amount of information that women don’t have, you know, could fill a room. It’s, it’s amazing. So, I am, I am passionate about it, because I think that again, we deserve to age healthfully. We deserve to go through our midlife. And let me say we spend a lot of time talking about, you know, the bad things or the negative things that happen to women in midlife. I’m here to tell you that midlife and beyond and particularly once you’re menopausal, I think that is where you have the opportunity to, to really live your best life, once you are freed from a lot of the responsibilities that saddle you in midlife, all those things that we talked about. And now for the first time in life, you get to pay attention to you, I get to do what I want to do. That’s a beautiful thing. So I think it’s something that we have to reframe this conversation, and have women understand that this is not something to dread. This is something really to look forward to, and anything and everything that you can do, to make sure that you feel good and are functioning properly at this point in your life is something that you need to make sure that you put in your tool bag.
Katie Vernoy 33:46
You’ve written a book that is part of this effort to get the word out. Can you tell us a little bit more about it?
Dr. Sharon Malone 33:52
Yes, I wrote my book is called Grown Woman Talk. And it’s really not just about menopause. And perimenopause is metaphoric, that’s a sliver of the book. It really was born of the notion that I am the only doctor in my friend group. And I’m the only doctor in my family. So, as such, I spend a lot of time navigating and negotiating people’s various and sundry healthcare issues. And the recurring thing that keeps coming up, that kept coming up again and again, was how little people understand how the system even works, you know, and or I talked to someone and they would ask me a question. And I would say, Did you doctor not tell you that? I’m confused as to why you don’t know that. And so the book is full of practical advice. There’s some medical advice. There’s a lot of storytelling because I think that that’s really how we sort of absorb information. But it starts with things like how to pick a doctor. What’s important, what’s important about your medical history, your family history. So there’s some logistical things that I think that people don’t get, because you have to understand the practice of medicine has changed. The locus of control now is not your doctor, who’s going to your nice, wonderful doctor who is going to give you great advice for the next 25 or 30 years. That’s not going to happen. You’re in control of your health. And that’s what I that’s the message I want women to get. And for those of you who might remember, there’s, there’s this book in the that was out in the 90s, when I was having my children called What to Expect When You’re Expecting?
Katie Vernoy 35:38
Yep.
Dr. Sharon Malone 35:39
Well, this book is what to expect when you expect to live beyond 40. It’s all the other other things, you know, and then we talk about some things that happen that you might expect in midlife, that may happen: fibroids, cancer, you know, high blood pressure, diabetes, we talk about those things. But ultimately, it’s to give you a navigational tool. And the earlier you read the book, the better. I it’s just like that window of opportunity. You know, there’s never a time that it’s a bad time to read it. But the earlier you are when you see things coming, and you’re like, Oh, well, that’s not surprising. And you know how to prepare for it and what to do if and when these situations come up. So that’s the book and the book. Sometimes I say, you know, we talk about some tough stuff; when you talk about cancer, and you’re talking about Alzheimer’s disease. But there I hope that through storytelling, and I do tell a lot of stories, a lot of family stories, I try to interject a little humor from time to time. And in the text, and at the end of each chapter, there’s a playlist. So it has a musical accompaniment at the. So…
Katie Vernoy 36:57
That’s amazing.
Dr. Sharon Malone 36:58
So when it feels like it’s gotten a little tough, then you can just go and go to Spotify or Apple and listen to my playlist and because I’m a closet DJ in my spare time.
Katie Vernoy 37:09
That’s amazing.
Curt Widhalm 37:11
Where can people find your book and find out more about you and the things that you’re doing?
Dr. Sharon Malone 37:16
Sure, you can follow me on Instagram. And my instagram handle is SMaloneMD. My website is Dr. D-R Sharon Malone.com. Go to my website lot of information about my book, and you can buy my book wherever books are sold, Amazon, Barnes and Noble, Walmart, Target every place. And all the links are provided in my weds website at DrSharonMalone.com.
Curt Widhalm 37:45
And we will include links to all of those in our show notes over at mtsgpodcast.com. Follow us on our social media join our Facebook group to continue on this conversation. And not only for our women clinicians, but also for all of our men out there. There’s plenty of benefits to learning about what’s going on with women in your life. So make sure that they listen to this episode as well. And until next time, I’m Curt Widhalm with Katie Vernoy and Dr. Sharon Malone.
… 38:16
(Advertisement Break)
Announcer 38:16
Thank you for listening to the Modern Therapist’s Survival Guide. Learn more about who we are and what we do at mtsgpodcast.com. You can also join us on Facebook and Twitter. And please don’t forget to subscribe so you don’t miss any of our episodes.




SPEAK YOUR MIND