What Therapists Should Actually Do for Suicidal Clients: Assessment, safety planning, and least intrusive intervention
Curt and Katie chat about suicide assessment, safety planning, and how to keep clients out of the hospital. We reviewed the Integrated Motivational Volitional Model for Suicide, we talked about what therapists should be assessing for in every session, what strong assessment looks like (and suggested suicide assessment protocols), and why the least restrictive environment is so important when you are designing interventions and safety planning. This is a continuing education podcourse.
Click here to scroll to the podcast transcript.Transcript
In this podcast episode we talk about suicide assessment, safety planning, and intervention
We continue our conversation on suicide, progressing from risk factors (from last week’s episode) to how to assess and safety plan with the least intrusive interventions at the earliest stages.
Review of the Suicide Model: Integrated Motivational Volitional Model by O’Connor and Kirtley
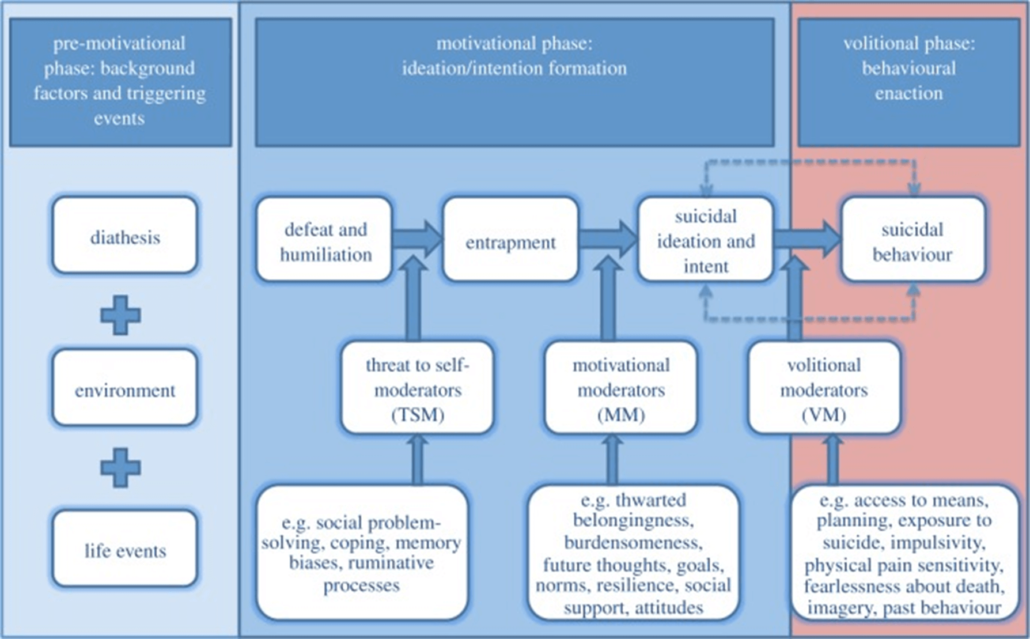
- Continued to review the IMV model
What should therapists assess for in every session, related to suicide?
“When clinicians are burnt out, when we have caseloads that are too big, when we aren’t taking care of ourselves, we tend to [think], “Okay, this client is at a six, they can live at a six for a while,” which is absolutely true. And if they can [live with this level of suicidality], and they have the good factors that allow them to live there – great. It’s just how close are they to that 7, 8, 9?” – Curt Widhalm, LMFT
- Moderating motivational factors, which move clients from passive to more active suicidality (or the reverse)
- Looking at what is keeping someone from being at risk for suicide (protective factors)
- The importance of knowing our clients well before they move into the volitional phase
- Understanding the clinician factors and putting structure around assessment
Assessment for Suicide
“Assessment is intervention.” – Curt Widhalm, LMFT
- SAMHSA’s GATE protocol
- Gather information using a structured assessment tool (Columbia Scale, LRAMP)
- Looking at intention, means, plan as well as risk and protective factors
- Moving into a safety plan
- The importance of recognizing the human during the assessment (versus focusing only on the protocol or your liability)
- Seeking supervision or consultation – don’t do this alone
The importance of using the least restrictive intervention for suicide
“There is a rupture in the therapeutic relationship when you are sending your client or facilitating a hospitalization against their will. It can save their lives …but that may not always be the case.” – Katie Vernoy, LMFT
- The idea of “responsible” action
- The range of options for keeping a client safe
- Having a conversation with the client on how to avoid attempting suicide
- The potential impacts of hospitalization, including trauma
- The danger of hospitalizing someone who does not need this level of intervention
- Additional intervention between sessions
- The practicalities to set up your schedule and your practice to support your clients and your self
- Additional risk factors (transition phases between providers)
Our Generous Sponsors for this episode of the Modern Therapist’s Survival Guide:
Thrizer
Thrizer is a new modern billing platform for therapists that was built on the belief that therapy should be accessible AND clinicians should earn what they are worth. Their platform automatically gets clients reimbursed by their insurance after every session. Just by billing your clients through Thrizer, you can potentially save them hundreds every month, with no extra work on your end. Every time you bill a client through Thrizer, an insurance claim is automatically generated and sent directly to the client’s insurance. From there, Thrizer provides concierge support to ensure clients get their reimbursement quickly, directly into their bank account. By eliminating reimbursement by check, confusion around benefits, and obscurity with reimbursement status, they allow your clients to focus on what actually matters rather than worrying about their money. It is very quick to get set up and it works great in completement with EHR systems. Their team is super helpful and responsive, and the founder is actually a long-time therapy client who grew frustrated with his reimbursement times The best part is you don’t need to give up your rate. They charge a standard 3% payment processing fee!
Thrizer lets you become more accessible while remaining in complete control of your practice. A better experience for your clients during therapy means higher retention. Money won’t be the reason they quit on therapy. Sign up using bit.ly/moderntherapists if you want to test Thrizer completely risk free! Sign up for Thrizer with code ‘moderntherapists’ for 1 month of no credit card fees or payment processing fees! That’s right – you will get one month of no payment processing fees, meaning you earn 100% of your cash rate during that time.
Simplified SEO Consulting
Have you spent countless hours trying to get your website just right and yet, it’s not showing up on Google and it doesn’t seem like anyone’s able to find it? Simplified SEO Consulting has a unique solution. They’ve been training therapists to optimize their websites, so they show up better on Google for the past 4 years. But let’s face it, with the busy schedules we all keep it can be hard to find the time to optimize your website even when you learn how. So, they are hosting a 16 day cruise in July 2023 going from LA to Hawaii and back. When you join them, you’ll get intensive SEO education and coaching during the 10 days at sea. Most importantly, you’ll have plenty of time to sit next to the pool and implement everything you’ve learned and then ask their team for feedback. Yes, it’s the perfect excuse for a Hawaii vacation. But it’s also a time to both learn about SEO and actually implement what you learn.
The upcoming cruise is a unique opportunity to learn to optimize your own website, have time to practice what you learn and the ability to get feedback from leading SEO professionals in our field.
To reserve your spot before it fills up, go to https://simplifiedseoconsulting.com/training-cruise-for-better-seo/
Receive Continuing Education for this Episode of the Modern Therapist’s Survival Guide
Hey modern therapists, we’re so excited to offer the opportunity for 1 unit of continuing education for this podcast episode – Therapy Reimagined is bringing you the Modern Therapist Learning Community!
Once you’ve listened to this episode, to get CE credit you just need to go to moderntherapistcommunity.com/podcourse, register for your free profile, purchase this course, pass the post-test, and complete the evaluation! Once that’s all completed – you’ll get a CE certificate in your profile or you can download it for your records. For our current list of CE approvals, check out moderntherapistcommunity.com.
You can find this full course (including handouts and resources) here: https://moderntherapistcommunity.com/courses/what-therapists-should-actually-do-for-suicidal-clients-assessment-safety-planning-and-least-intrusive-intervention
Continuing Education Approvals:
When we are airing this podcast episode, we have the following CE approval. Please check back as we add other approval bodies: Continuing Education Information including grievance and refund policies.
CAMFT CEPA: Therapy Reimagined is approved by the California Association of Marriage and Family Therapists to sponsor continuing education for LMFTs, LPCCs, LCSWs, and LEPs (CAMFT CEPA provider #132270). Therapy Reimagined maintains responsibility for this program and its content. Courses meet the qualifications for the listed hours of continuing education credit for LMFTs, LCSWs, LPCCs, and/or LEPs as required by the California Board of Behavioral Sciences. We are working on additional provider approvals, but solely are able to provide CAMFT CEs at this time. Please check with your licensing body to ensure that they will accept this as an equivalent learning credit.
Resources for Modern Therapists mentioned in this Podcast Episode:
We’ve pulled together resources mentioned in this episode and put together some handy-dandy links. Please note that some of the links below may be affiliate links, so if you purchase after clicking below, we may get a little bit of cash in our pockets. We thank you in advance!
SAMHSA’s TIP with the GATE Protocol
COLUMBIA-SUICIDE SEVERITY RATING SCALE
LINEHAN RISK ASSESSMENT AND MANAGEMENT PROTOCOL (LRAMP)
References mentioned in this continuing education podcast:
Carmel, A., Templeton, E., Sorenson, S. M., & Logvinenko, E. (2018). Using the Linehan Risk Assessment and Management Protocol with a chronically suicidal patient: A case report. Cognitive and Behavioral Practice, 25(4), 449-459.
Goldman-Mellor S, Olfson M, Lidon-Moyano C, Schoenbaum M. Association of suicide and other mortality with emergency department presentation. JAMA Netw Open. 2019; 2(12):e1917571.
Interian, A., Chesin, M., Kline, A., Miller, R., St. Hill, L., Latorre, M., … & Stanley, B. (2018). Use of the Columbia-Suicide Severity Rating Scale (C-SSRS) to classify suicidal behaviors. Archives of suicide research, 22(2), 278-294.
Linehan, M. M., Comtois, K. A., & Ward-Ciesielski, E. F. (2012). Assessing and managing risk with suicidal individuals. Cognitive and Behavioral Practice, 19(2), 218-232.
Pinals, D. A. (2019). Liability and patient suicide. Focus, 17(4), 349-354.
Posner, K., Brent, D., Lucas, C., Gould, M., Stanley, B., Brown, G., … & Mann, J. (2008). Columbia-suicide severity rating scale (C-SSRS). New York, NY: Columbia University Medical Center, 10.
Substance Abuse and Mental Health Services Administration (US); (2009. Addressing Suicidal Thoughts And Behaviors in Substance Abuse Treatment [Internet]. Rockville (MD): (Treatment Improvement Protocol (TIP) Series, No. 50.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK64022/
*The full reference list can be found in the course on our learning platform.
Relevant Episodes of MTSG Podcast:
Part 1: Risk Factors for Suicide: What therapists should know when treating teens and adults
Rage and Client Self-Harm: An interview with Angela Caldwell
Who we are:
 Curt Widhalm, LMFT
Curt Widhalm, LMFT
Curt Widhalm is in private practice in the Los Angeles area. He is the cofounder of the Therapy Reimagined conference, an Adjunct Professor at Pepperdine University and CSUN, a former Subject Matter Expert for the California Board of Behavioral Sciences, former CFO of the California Association of Marriage and Family Therapists, and a loving husband and father. He is 1/2 great person, 1/2 provocateur, and 1/2 geek, in that order. He dabbles in the dark art of making “dad jokes” and usually has a half-empty cup of coffee somewhere nearby. Learn more at: http://www.curtwidhalm.com
 Katie Vernoy, LMFT
Katie Vernoy, LMFT
Katie Vernoy is a Licensed Marriage and Family Therapist, coach, and consultant supporting leaders, visionaries, executives, and helping professionals to create sustainable careers. Katie, with Curt, has developed workshops and a conference, Therapy Reimagined, to support therapists navigating through the modern challenges of this profession. Katie is also a former President of the California Association of Marriage and Family Therapists. In her spare time, Katie is secretly siphoning off Curt’s youthful energy, so that she can take over the world. Learn more at: http://www.katievernoy.com
A Quick Note:
Our opinions are our own. We are only speaking for ourselves – except when we speak for each other, or over each other. We’re working on it.
Our guests are also only speaking for themselves and have their own opinions. We aren’t trying to take their voice, and no one speaks for us either. Mostly because they don’t want to, but hey.
Stay in Touch with Curt, Katie, and the whole Therapy Reimagined #TherapyMovement:
Consultation services with Curt Widhalm or Katie Vernoy:
Connect with the Modern Therapist Community:
Our Facebook Group – The Modern Therapists Group
Modern Therapist’s Survival Guide Creative Credits:
Voice Over by DW McCann https://www.facebook.com/McCannDW/
Music by Crystal Grooms Mangano https://groomsymusic.com/
Transcript for this episode of the Modern Therapist’s Survival Guide podcast (Autogenerated):
Curt Widhalm 0:00
This episode of The Modern Therapist’s Survival Guide is brought to you by Thrizer.
Katie Vernoy 0:03
Thrizer is a modern billing platform for private pay therapists. Their platform automatically gets clients reimbursed by their insurance after every session. Just by billing your clients through Thrizer you can potentially save them hundreds every month with no extra work on your end. The best part is you don’t have to give up your rates they charge a standard 3% processing fee.
Curt Widhalm 0:24
Listen at the end of the episode for more information on a special offer from Thrizer.
Katie Vernoy 0:29
This episode is also brought to you by Simplified SEO Consulting.
Curt Widhalm 0:33
Have you spent countless hours trying to get your website just right and get it’s not showing up on Google and it doesn’t seem like anyone’s able to find it. Simplified SEO consulting has a unique solution. They’ve been training therapists to optimize their websites, so they show up better on Google. But let’s face it with the busy schedules we all keep it can be hard to find time to optimize your website even when you learn how. So they’re hosting a 16 day cruise in July 2023 going from LA to Hawaii and back. When you join them, you’ll get intensive SEO education and coaching during the 10 days at sea. Most importantly, you’ll have plenty of time to sit next to the pool and implement everything you’ve learned and then ask their team for feedback. Yes, it’s the perfect excuse for Hawaii vacation, but it’s also time to both learn about SEO and actually implement what you learn.
Katie Vernoy 1:24
Listen at the end of the episode for more information on Simplified SEO Consulting,
Announcer 1:29
you’re listening to The Modern Therapist’s Survival Guide where therapists live, breathe and practice as human beings. To support you as a whole person and a therapist, here are your hosts, Curt Widhalm and Katie Vernoy.
Curt Widhalm 1:45
Hey, modern therapists, we’re so excited to offer the opportunity for one unit of continuing education for this podcast episode. Once you’ve listened to this episode, to get CE credit, you just need to go to moderntherapistcommunity.com, register for your free profile, purchase this course, pass the post test and complete the evaluation. Once that’s all completed, you’ll get a CE certificate in your profile, where you can download it for your records. For a current list of our CE approvals, check out moderntherapistcommunity.com.
Katie Vernoy 2:16
Once again, hop over to moderntherapistcommunity.com For one CE once you’ve listened.
Curt Widhalm 2:18
Welcome back modern therapists and back to part two of The Modern Therapist’s Survival Guide continuing education episode on suicide, intervention, assessments, all of this kind of stuff. If you have not yet listened to part one, go back to part one, because it’s going to be referenced here from the very top of this episode. And we’re picking up more or less where we left off. But in the last week, since you’ve all joined us, we have regrouped. We’re ready and re-energized for part two. Katie’s head is in her hands. She is not energized about this, talking more about working with clients who are suicidal. And we are picking right back up really starting to take what we’ve taught as far as risk factors. And walking us through how clients who are presenting with this according to the model, where we need to intervene at the right time in order to be able to most effectively help our clients not jumping straight to, you know, the big, bad, scary parts of things, but picking up on a lot of the motivational factors that show up with clients who are presenting with suicidality.
Katie Vernoy 3:35
Again, we’re talking about suicide. So just be aware. I think it’s something where, as we talked about last episode, I think it’s really important that we keep having these conversations. And if you’re not in the right space to listen today, please come back and listen another day. I find that there, and we’ve talked about this Curt, I’ve found that there’s a lot of folks who think they know what to do about suicide, but may actually be making things worse. And so we want to talk about how you can help your clients that are dealing with suicidality, maybe those who’ve had previous attempts and help them to avoid hospitalization, suicide attempts, suicide completion, all of those things. This is a really important conversation.
Curt Widhalm 4:20
As a reminder, the IMV model of suicidality the integrated motivational volitional model, developed by Rory O’Connor and further updated by O’Connor and Olivia Kirtley is a three factor model that looks at the pre-motivational phase and background factors and triggering events, the motivational phase and the volitional phase of suicidality. We in our first episode had covered the pre-motivational phase, the diathesis, environment, life events. We were partway through the motivational phase talking about feelings of entrapment that come out of threat to self and defeat and humiliation, social problems, coping problems, those kinds of things leading to rumination and that kind of stuff. And there’s another piece of this before we get to the volitional phase, which is the actual suicidal behavior piece of where people are taking actions. And we’ll get to that here in a little bit. But wanting to wrap up the motivational phase, this is where the ideation and the intention start getting formed. When our clients are in that feeling of entrapment, they can’t see what other options might be available to them. They’re really starting to ruminate on stuff, they might have some of those sensitivities to feelings of flooding. This is where we want to talk about the motivational moderators as defined by a O’Connor here. And I think that this is a piece of the ongoing suicidal assessments that all clinicians need to be really aware about. Because this is the phase where we can often overlook a lot of the early symptoms of what people who are on the pathway to suicidal behavior started exhibiting beyond kind of those classic, you know, pop culture, sort of like taking care of their affairs and giving away belongings and that kind of stuff. But this is really being able to listen to the negative motivational moderators, feelings, like burden sums, or being a burden on other people. Feelings of making attempts to belong to other groups, and those feelings being thwarted. The absence of any sort of resilience, the absence of thoughts about the future, these kinds of things are things that we should be assessing every client in every session for. This is kind of that soft suicide assessment sort of thing of, are we hearing motivational moderators that are tipping, if you know, the right circumstances end up happening for a client that will trigger kind of a passive suicidal ideation into here’s a motivating factor that pushes us into that suicidal behavior. And what that allows us to do is also really reinforce the positive moderators here, hey, you’ve got a great social support group here that, you know, they tend to really show up for you even when you don’t say that they do, or when you’re feeling left out, like, whenever you ask, they do show up. Really being able to build positive moderating factors here as well.
Katie Vernoy 7:49
To me, when you’re describing it, it really sounds like a description of what therapy looks like. I mean, when I look at it, I mean, when we’re when we’re interacting with clients, and we’re trying to help them get to wherever they want to go, and even if this is personal growth, anything down to like, My life sucks, and I, I don’t see any way out, you know, all of that. I think we’re constantly assessing these things. And to me, and maybe this is having been a therapist for almost half my life. But I think there’s that element of when someone is getting into this space, where they the entrapment space when they start expressing some of these things of hopelessness, feeling like they’re a burden, feeling completely isolated, or ostracized, not feeling that they have things to look forward to, you know, and we can, you know, kind of just reference the risk factors and kind of tie back to the first episode where we talk about risk factors and protective factors. But to me, I’m always looking at this stuff and I get that pit of the stomach feeling when someone starts getting into that entrapment and, and some of these also, motivational moderators are things that impact their motivation for living I would assume is kind of what we mean by motivational moderators. Like I just feel it I feel this hopelessness, this kind of devastation or giving up or whatever it is, like, it feels like it’s something that comes across in the room, across the screen, whatever it is, but going beyond that feeling and actually doing assessment feels important, especially when you’re talking about like, anyone can be in this space. But to me, it just it feels like this is what I do in therapy is trying to assess these things and help them to improve the quality of their life by having positive motivational moderators or protective factors. In our conversations you’ve said that the people don’t do this well. or miss these things. But to me, it feels organic. So I feel like there’s probably things that I’m missing here. And so I just want to kind of make sure that we’re being really specific to what exactly these conversations look like. Because to me, it feels like, organically, these conversations are already happening,
Curt Widhalm 10:18
As you’re pointing out, what you’re describing is good therapy. And, while I think a lot of seasoned clinicians and especially clinicians who have worked with high risk populations before tend to find themselves pulled more naturally into doing things that work. And especially when they’ve been successful in the past. I think that when I hear clinicians, and frankly, even in some of the earlier parts of my career, where I wasn’t supervised or trained properly on this, is that I’ll admit to being a lazy clinician at times, and I see and hear this from, you know, some of the clinicians that I talk with in the community, I make a point to bring this up in supervision and this kind of stuff, make sure that you’re emphasizing a response to these kinds of statements from clients, because these are the kinds of things that retro-actively four or five, six sessions later where you see a client on the decline, that you’re laying the foundation, four, we’ve already put in these positive motivational factors, these resilience factors of being able to rely on other people for help. That we can ask for help. Because it’s not like clients wake up one day and are just like, you know, what, today’s the day that I’m going to be suicidal. That, especially for some of these more slow burn sort of build ups of feelings of isolation, or rejection from social groups. Or, when we talk about the risk factors, when some of that negative motivational factor sort of things already happens in I’m feeling like a burden on other people, but I can rely on my wife. Where you know, if that wife ends up, dying in an accident, or leaving the relationship all of a sudden, where there’s that extra triggering risk factor that’s present, if the clients are already in that entrapment phase. This is where, yes, we probably a lot of us are kind of doing this in general. But making sure that we’re listening earlier for this could be several steps ahead of a suicidal risk ideation sort of process. And I think where I’m trying to emphasize this over the last episode, in this episode is that we as a field should be thinking more in terms of more of our clients are at risk for suicide than we actually believe that they are, and that we really need to be focusing on Is there potential for suicide with these clients, because the numbers of suicide attempts and suicide completions are going up. And we as a field are facing people coming in at all risk levels. And really, frankly, anybody is eventually at a risk for it. But if we can do these earlier interventions, even if it’s not the clients goals already, you know, upon coming in. Still continuing to emphasize what amounts to a really good bio psychosocial sort of overlay across all of the treatment plan.
Katie Vernoy 13:42
That makes sense. I think, for me, the the piece that I’ve probably missed in the past or the things that I haven’t necessarily been so good at when I especially when I’m burned out, and I’m not remembering things, right, is that I’ve I’ve been either afraid to kind of delve deeper into some of the hopelessness, and I think, you know, and all of the conversations we’ve had about suicide, that’s something where it’s like, ask, don’t hesitate, ask, even if it’s, if it feels a little bit like a leap, the client may appreciate it. And it may have been a window or a door or whatever, to have a better conversation or a deeper conversation. But I think when I, when I look at what we’re actually asking clinicians to do here, we’re asking them to really know their clients well.
Curt Widhalm 14:33
Yes.
Katie Vernoy 14:32
And understand what motivates them what they see as connecting who, who they actually can really rely on what they what they feel like their value might be or are building that self worth and value. So that we we actually are, are addressing these things because for one person, being able to have some time in solitude, and having some online relationships, for example is very nourishing and for someone else that would be a sign of isolation, and potentially social disconnection. And so really understanding our clients and where they fit on all these different things in their unique situation, the animals and humans in their life, their loved ones, all of that, so we can really get a sense of it. It feels really important. And we either have to take copious notes for ourselves, so that we can remember all these things, or we need to be really present. So we, we lock it into that kind of array of memories, and, and that kind of portrait, the inner portrait we have of our client, so that we know like, hey, this client doesn’t take care of themselves when these types of things happen, or this client doesn’t do things, when this happens, or this client gets really hopeless when they interact with this family member, or whatever it is, we have to know those things. And I think when I was really burned out, and I would forget things and had a lot of clients with a lot of similar stories, there’d be times when I would not recognize a warning sign. And so I think it is important to kind of be really aware of how important this information really is.
Curt Widhalm 16:09
And I’m gonna come back to a couple of points that you’re talking about here, when we get to the need for some of the assessments and the way that we do them. And I want to just finish covering kind of this IMV model here a little bit first. So that way we can close out this part of it. What those motivational moderators do is they take that suicidal ideation and intent, and they turn that into suicidal behavior. And I think where a lot of the traditional education that we get on intervening with suicide focuses on this volitional behavior piece of it, this is limiting the access to the means to make their attempts. This is when you see kind of those traditional things that you know, taking care of affairs sort of things, you know, the exposure to other suicide, impulsivity factors, fearlessness about death. At least early on in my career, and a lot of the more basic trainings that I’ve seen around suicide interventions have focused solely on this phase. And this is why I placed so much emphasis on that moderating factors, moderating motivators phase, because if we can prevent even getting to this phase, we’re a lot more likely to be successful in helping intervene with our clients, at the least restrictive means necessary. But a lot of what ends up happening and kind of, oh, a client has died by suicide, or we see, you know, whoever it is in the news has died by suicide, we kind of retro actively go back and be like, Oh, here’s this thing in common that happened here. This is why we’re going to, you know, encourage people to give up their firearms or do not have the stockpile of medications that they have, or if it’s a client who lives on a high floor of an apartment complex, or a condo, that we get them to stay with a family member, where it takes out risks of things like jumping. And so, you know, those are things where, if we are really paying attention earlier to the motivational moderators, we should already know, kind of the risk factors that really put things in that volitional phase because once those moderating motivators end up going to that negative side, that’s when it’s the true crisis situation. Not that the rest of suicidality isn’t a crisis situation, but it gives us a lot better time to be able to intervene earlier and know what’s essentially ongoing risk factors and why we need to continue to at least passively, but really more often, actively ask about suicidal ideation and the risk factors that go along with it.
Katie Vernoy 19:04
What I see frequently is this passive suicidality, and I know that that we’re not talking necessarily about that, but but I feel like in this kind of motivational phase, there’s a lot of passive suicidality. And I have a lot of folks that will say, you know, I don’t want to die, but I don’t care if I live. And I think that those when I start hearing those kinds of conversations, I really try to start digging into these other factors and address it there. Not like Whew, don’t have to do a whole safety plan. It’s that element of okay, this is someone that is not actively suicidal, they’re starting to have some of these hopelessness and treatment kind of feelings, but they’re not taking steps yet. Okay, let’s let’s intervene here. Before someone gets to, well, I don’t want to I don’t want to die by suicide today, or I don’t want to take my life today. But I can’t promise tomorrow, right? Like when we when we start moving into like, okay, there’s some behaviors here. Yes, we need to do kind of the traditional assessment for means and those types of things. But when we’re still at this kind of like, I just, you know, yeah, I’m not suicidal, but I just, I don’t care if I live, you know, like, I’m just, I’m making it through day by day, but I just don’t care. I just don’t think it’s gonna get better, or I don’t think I’m ever gonna get better. I think those conversations, to me are things that we intervene with. But I think recognizing that this is something that can escalate.
Curt Widhalm 20:35
I mean, the very blunt way of saying it’s with clients like this, it not to the clients like this, but the very blunt way of saying it is like, Okay, if a client’s here, what would it take to move them into that very active phase? Like, is it this extra additional thing, and working against whatever those potential things are in that phase. And I think that when clinicians are burnt out, when we have case loads that are too big, when we aren’t taking care of ourselves, we tend to kind of stow it away in our minds as far as like, Okay, this clients at a six, they can live at a six for a while. Which is absolutely true. And if they can, and they have the good factors that allow them to live their – great. It’s just how close are they to that 7, 8, 9. And that’s the part that I think, especially with depressed clients, that kind of can make it feel very laborious in session to do a lot of the lifting of the energy for clients. It gets hard if you are not following an assessment plan, and you’re not following a safety plan. And this is where to help with some of the clinician factors that you were mentioning earlier, why I like having good robust assessment plans, and good safety plans, because it relies less on us remembering all of this stuff, and it gives us something to follow so that way, we’re not forgetting it. That makes sense. And I’m going to frame this out of SAMSA’s approach to working with suicidality. And we’ll include this link in our show notes over at mtsgpodcast.com. But they have what’s called the GATE approach. And the first step of this is gather information. And well, a lot of us as good clinicians will be taking copious observations of our clients. Part of what I really recognized about our field, when it comes to recognizing and intervening with suicide is, we’re in our infancy on this. We have been really bad about this for a very long time, and are just now starting to really end up with good assessment and good intervention tools. And we’ve talked in one of our kajillion episodes before about some of the things that, you know, we were taught earlier in our careers. And I think one of the gold standards that has emerged over the last 10 years or so is the Columbia-Suicide Severity Rating Scale. And this is a oftentimes, you know, two to three page kind of questionnaire that you ask clients if there’s certain factors that are present in their lives, and how severe on a scale of 1 to 10 that those feelings have been not only recently, but within the last six months. And I have found this to be a pretty good snapshot in time of where clients are at a particular moment. And while it does look a little bit historically at where a client’s feelings have been. Taking advantage of knowing what risk factors are and being able to follow a protocol so that way, you’re not sitting there being like, hey, what was it that Curt and Katie said on that award winning podcasts about this? Am I remembering all of the risk factors. That they’re at least written down in front of you to kind of go through a checklist because when we get stressed out and especially early in our careers, when we’re first having a client sit in front of us with suicidal thoughts. We start to freak out it’s scary working with people who want to die. And when we get into that big limbic system activity in our own selves, we start forgetting to do stuff and this is where it’s great to have a protocol that you can pull out and not miss much. Now, there is no protocols out there that 100% predict suicide. There is no protocols or assessments or anything. You are an active part of this. You are part of the assessment process. You are one of the tools. Yes, I’m calling our listeners tools. But this is where not relying on, I need to pull into my deep memory and remember everything. There is no shame in being able to use something that guides you through keeping your clients alive.
Katie Vernoy 25:23
Sure. And I think the point that I want to amplify just really quickly is that these are tools that provide you with the questions to ask, and a little bit of feedback on what those answers mean. It’s, it’s an assessment tool, but I almost feel like it’s an intervention as well, because you’re actually it’s guiding a conversation. And like I said, these conversations are the thing of therapy. And so to me being able to have that guided with something that’s backed with, hopefully, a little bit of research and, you know, best practices, I think those things can be very helpful. And do not over rely on them to predict suicide, it’s, they are helping you get the information you need to make that assessment.
Curt Widhalm 26:14
And as I stated in the last episode, assessment is intervention. And especially talking in the IMV model of where we’re looking at clients. That if we’re taking the background information, and we’re continuing to assess in that pre motivational phase, great. You’re intervening at the right level for where clients are at.
Katie Vernoy 26:42
Yeah.
Curt Widhalm 26:43
And if you’re intervening at the level of the motivational phase, where there’s ideation starting to form, that is the right level. And I’m going to continue to emphasize we want to come to the least restrictive level of intervention necessary. And if that’s, you know, an intervention like, hey, you know, you should really call your friend that you haven’t talked to in a couple of weeks.
Katie Vernoy 27:09
Yep.
Curt Widhalm 27:11
Then that is a great suicide prevention technique.
Katie Vernoy 27:15
Yes. So you have mentioned in other conversations that the Columbia scale is one that you use, but you prefer the LRAMP.
Curt Widhalm 27:28
The LRAMP. Yes. I find that while the Columbia scale is a good snapshot, it is something that only helps to identify the risk factors and what’s going on. It does not help us to have a conversation that naturally builds into a safety plan. It doesn’t help us to, it relies on clinicians to then be able to take the information from this assessment and put it into something else that a client can walk away with and be like, Okay, here’s, here’s a good safety plan here. And this is why I do like the Linehan Risk Assessment and Management Protocol, developed by the wonderful Marsha Linehan, it’s shortened down to the LRAMP. And this is a little bit more robust treatment planning out of this as well, because while it’s semi structured, it makes you cover a lot of the risk factor areas, but it also makes you come up with the client, a safety plan, that they are invested into having created. It’s not just somebody being like, here’s things that you should do, or horribly, you know, clinicians that still are like, Here, sign this no harm contract. But it’s wonderful, you know, let’s look at acute risk factors, you know, is there a current suicide plan? Well, I need to ask my client now, do you have a current plan to die by suicide or to make a suicide attempt? If so, what is it? What is your preferred method? What’s currently or easily available to you? It also helps us to identify protective factors. And again, if we go back to this entrapment discussion, this is starting to build that reasons for living that, you know, hey, you do have some of these things going on. Or if you don’t, this helps us to identify specific ways to start reaching some of these protective factors that can help in the overall treatment picture of working against some of those risk factors. What it also does is helps us into looking at treatment actions based on the chain of events that have led to this specific moment. And you know, there’s it’s Marsha Linehan it’s DBT related stuff, but it’s…
Katie Vernoy 29:59
So there’s a chain analysis built into this LRAMP thing?
Curt Widhalm 30:03
Yes, there is.
Katie Vernoy 30:05
All right.
Curt Widhalm 30:07
You sound less than enthused about this.
Katie Vernoy 30:10
I mean, I think for folks that don’t like DBT, they may not be, they may or may not be excited about this, but I, I’ve always, you know, appreciate it elements of DBT. So I think it’s fine. I just, you know, it’s something where do you have to learn how to do a proper chain analysis to use the LRAMP?
Curt Widhalm 30:32
It’s better than a dead client. And it’s, and it’s better than doing absolutely nothing at all. But if you go back to looking at, how did you get into this, a lot of times what that leads to, even if you’re doing kind of a half assed chain analysis, full asset people, but if you don’t do it great, like…
Katie Vernoy 30:56
If you haven’t been trained on DBT, is what you’re saying, you can still do, you can partial ass…
Curt Widhalm 31:02
Yes.
Katie Vernoy 31:04
…chain analysis, okay.
Curt Widhalm 31:07
But what this does is helps to identify in this phase, what are the particular vulnerability factors that led to this. And what that does is, in the short term, helps you to be able to address those vulnerability factors, but in the long term, helps you to build more resilience against those vulnerability factors in the long term. And gives us a pretty good idea of if there is suicidal ideation returning what a client’s pathway to that ideation is likely to be based on the past events.
Katie Vernoy 31:41
So when you’re talking about that, the thing I’m picturing is the bazillion conversations I’ve had with clients, where I just organically asked how did this happen? Right? Like, you know, that’s a CBT thing. It’s a DBT thing. It’s a therapy thing, right? Like, let’s go back in time, let’s let’s walk through, when was the last time you didn’t feel this way. And then when you started feeling this way, you know, like what was going on. And at times, this is where I’ve identified like, the person was extremely dehydrated or hadn’t slept for a while, or that was the day after they lost their job, or whatever it is. And I think oftentimes, it helps to pull folks out of that tunnel vision entrapment space, because they recognize that this is something that was triggered versus something that just has always been this way. And it also I think, helps me to identify some of the things that will trigger and some of the things that might quickly be able to transform this feeling going forward. And so to me, although I had the reaction about the chain analysis being inherent in this, it was more about worrying that people would be able to use it. But I think for me, knowing that part of this is truly an intervention that most of us might go to, to figure out Okay, what happened? And how rich the information is that you get from it, I think is very helpful. And I think those are the types of things where if this if a an assessment tool has built into it, the follow on interventions, I think it is very helpful, because you’re not pulling out tons of different pieces of paper. You’re not having to think about it on your own. I think at times, especially when you’re overwhelmed by someone’s suicidality, I think it can be very helpful to have some guidance. So this sounds good. I give my my vote of approval on this.
Curt Widhalm 33:38
Well, and to point out a couple of other things that I really like about this is it also builds in here, reminding you to validate the client’s current emotions. Because I think that sometimes when we’re, you know, swaying between, okay, we’re in crisis mode, and we need to respond and then getting overly rigid into the protocol of like, okay, I’m going to rely on this protocol. Oh, yeah, there’s also still a human here. I hadn’t this is I assume most of our modern therapists are going to be good and warm people throughout this whole process. But let’s face it, there’s clinicians who aren’t and I think that this is something where if even if there’s built in reminders of like, you know, what, be a human in this part of the process. And, you know, I found myself talking in lecture to my line ethics class just yesterday about this that a lot of what are fields response to working with suicidal clients has been seemingly comes from reducing your liability in case something goes wrong. And I think that that’s led to a lot of what our responses in this field have been, which is to pass the client you know, and pass the buck on to somebody else, and why we are so quick to escalate to higher levels of care. But the final parts of the LRAMP is a checklist of was hospitalization considered? And if not why? Or it makes you go through kind of your thought process, and it’s built into your assessment right there. As far as here’s some of the legal protective factors that you might forget, and go ahead and do them. And that leads really well into your documentation. So that way, you’re not needing to document a lot. Just on top of everything else.
Katie Vernoy 35:36
Is this LRAMP available to everybody?
Curt Widhalm 35:42
We will put the one that is linked and available on the website and put that in our show notes. And we’ll deal with whatever lawyers and anything like that that come because we’re in the business of saving people.
Katie Vernoy 36:01
Well, my assumption is, if it’s on a public facing website, we we’re good to go.
Curt Widhalm 36:05
Yeah.
Katie Vernoy 36:06
In talking about the LRAMP, one more thing, before we move on to the next step step of this GATE approach. I am really struck by it, kind of setting the tone and getting through to a pretty good process. And I know that there are these additional motivating factors for clinicians, sometimes it’s like, hey, I want to get rid of my liability, like what you talked about with your lawn ethics class, another time for me, I was trying to do everything I could not to have to hospitalized someone because it was such a pain in the behind. Like, okay, what can I do? I didn’t want to have to sit there for hours waiting for an ambulance, I didn’t want to have to do all the additional paperwork. Like for me, I was actually motivated in the other direction. Because I didn’t, I didn’t I mean, I think there’s also reasons and we’ll talk about it that go into the hospital isn’t great. But like, for me, I think having a protocol in this regard, will allow for it to be a little bit more objective versus what the clinician is hoping for, like, hey, I want to put them in the hospital because I don’t want to deal with them. Or, hey, I want to keep them out of the hospital because the paperwork is a pain in the ass. So, so anyway, that’s the last thing on the LRAMP. But I know we need to continue on this GATE approach. So we’ve gathered information, that’s our G, what’s next?
Curt Widhalm 37:29
Access supervision.
Katie Vernoy 37:31
Okay.
Curt Widhalm 37:33
Found, one of the things that I love about our field is how we can cram any kind of acronym into anything else, whether it makes sense or not, but it’s accessing supervision. Don’t do this alone, that even when you are following a good protocol, whether it’s Columbia scale, whether it’s the LRAMP that accept that you might be missing things, and you want to talk with other clinicians, a supervisor, boss, somebody who has more experience in this stuff than you do. So that way, you make sure that you’re doing the right thing with your client, and that you’re not missing anything as far as your safety plan goes. That you’re able to really just work well with your client and not take this on fully yourself. This has the added benefit of working as a team and being able to have kind of other people to process through kind of what you’re working through in your own reactions to the clients in real time. Like, hey, I’m really stressed out about this. And I just kind of needed an extra set of eyes, that somebody is naturally able to kind of be like, Alright, are you taking care of yourself? Are you drinking water? Are you…?
Katie Vernoy 38:46
Yeah.
Curt Widhalm 38:46
You know, these kinds of things. So not doing this alone is really the big piece of this?
Katie Vernoy 38:52
How often would you say that you as a seasoned clinician, who is a supervisor yourself: How often are you accessing supervision or consultation when you’re doing a suicide assessment?
Curt Widhalm 39:04
I would say three quarters of the time.
Katie Vernoy 39:07
Okay. So reaching out to colleagues.
Curt Widhalm 39:11
And admittedly as my group practice is getting trained in DBT right now we have our team consultation set up each week where this is now becoming just more and more of, we’ve got that built into our schedule already, whether or not they’re suicidal clients who are present.
Katie Vernoy 39:31
That makes sense. I just was curious because when in how we talk about supervision versus consultation, it feels like it’s something that is an early stage career stage suggestion, but what you’re saying and I think how you and I both operate is when there’s something like this going on it’s really good to seek out a colleague, if you’re fully licensed, don’t have a supervisor, you have your own practice, to get a colleague that you can discuss these things with.
Curt Widhalm 39:59
Mm hm. T is take responsible action. And again, I’m going to come back to this phrase of least restrictive means necessary to intervene with the client. And this is where we’re going to look at hospitalization if hospitalization is necessary. If this is, you know, releasing to the care of parents, in the case of teenagers, that parents are able to say, Yeah, we understand that our child is having these thoughts. We’ll go home. We’ll take care of, you know, removing any access to means, this kind of stuff. That it’s being able to put the client in the right environment possible. And not anything that’s necessarily any more than what they need. And part of again, reaching out for supervision is if there’s other treatment team members, psychiatrists, school counselors, in the case of students, this kind of stuff, if. You have but one perspective, it’s an important perspective. But if there’s other people who identify other risk factors, that everybody is kind of being able to say, Okay, here’s why this client might be best for, you know, going to intensive outpatient treatment, rather than needing to go into a 72 hour hold situation. What they need is more opportunities to practice these skills in a structured environment, rather than a really expensive, really crappy but glorified hotel visit.
Katie Vernoy 41:35
Meaning hospitalization.
Curt Widhalm 41:37
Meaning a hospitalization. But it’s being able to do it in the way that is the necessary thing for a client.
Katie Vernoy 41:48
So I know we need to get into E at some point. But before we move on, I really wanted to sit here for a little bit if we can to really understand: How do how does someone get to what is the right level of care? What’s responsible action? And my experience, and you can tell me how close I am, is that when I was I was LPS designated being lanterman petris short, which was it’s a California thing where I was able to actually write a hold, and then they would go and get assessed again at the hospital. But what I would find in those conversations is that it was a conversation with a client. If a client wanted to get hospitalized, for example, oftentimes, there was nothing I could do to change that, you know, some, especially I think, some kids that were in the system, potentially in foster care, in homes where they were not safe at home, they would, they would seek hospitalization as a respite from their life. And so there were times when that was the case. And I think that’s a unique situation. But more typically, and the clients that I see now, and some of the clients I even saw then, it was something where if they didn’t want to go to the hospital, and we were having the conversation, it would help to really assess what they needed to remain safe. Now, if they absolutely could not agree to anything, then sometimes it was hospitalization against their will. And that handful of times like I rarely hospitalized folks, for the reason that I didn’t think it helped, as well for most clients, as well as the big pain in the ass of the paperwork. But for those times, when I when I had to do that, that was something where I really had to think through Is this the best, the most important thing? But short of hospitalization, it oftentimes became a really complex conversation about all of the resources, all of the protective factors, all of the things that could keep someone safe in that moment, and until the next contact that I had with them, in order, or the next contact that the therapist had with them if it wasn’t my client. And oftentimes it was very unique, what the quote unquote, least restrictive environment or responsible action would be. And so to me, it seems like it’s kind of this extension of being able to do good therapy, which is if you’re telling me or if I’m sensing that you’re suicidal, and we have this conversation, there is at least a part of you that does not want to die. And so working together to be able to resolve that seems important because my my sense of it, and this is something where definitely correct me if I’m wrong. My clients, if they want to die, they just aren’t going to come to therapy, and they’re just going to do what they’re gonna do. Whereas if they are if they’re ambivalent, or they don’t want to die, or a portion of them doesn’t want to die, they’re gonna come in and talk to me about it.
Curt Widhalm 44:40
I’ve got permission from a client to share the effects of a statement that was made after a hospitalization and a period of time afterwards. This client told me that in the moment that they were hospitalized they absolutely wanted to die, that it was something where they did not want to have the conversation, the team around this person at that time did initiate a 5150, this client was forcibly brought into the hospital, was all of the worst things were possible that were happening, and what this client has shared with me. And now, a few years after this experience is, how absolutely destroyed, they have been by how traumatic that whole process was. And that it’s not only was it being forced into the hospital, it was the most uncomfortable room that they’ve ever been in, it was being forced to take medications that they did not want to take, it was being woken up every couple of hours to make sure that they were still alive, and with some of the most uncaring, and just clinical people who are there and doing the best practices part of their job. And they absolutely hate every aspect of that part of their life. And they are thankful that it happened because they’re still alive now.
Katie Vernoy 46:16
Yeah.
Curt Widhalm 46:17
And I think that this is the thing that when I’m talking with clinicians, when I’m talking with clients about things is these moments when we get to a 5150, a, you know, hospitalizing clients against their will, that they’re in such a hyper focused state at that point that it does take a high level of intervention necessity. But it’s important to do that only with the clients who actually need to do that piece of it. And I think that that’s really the part that you’re bringing up here is in those clients who can see some of those, you know, alternate sort of ideas. That most clients with suicidal ideation, do end up surviving. And what they need is to be able to be put in the right kind of support to have the practical skills, and the practical supports necessary to deal with whatever is causing that crisis in that moment. And that’s really what we’re aiming for. And so some of these kids that you’re talking about who are escalating things, because it gets them out of a really bad home environment, and this is their hospital stay, it’s being able to use our permitted breaches of confidentiality to help intervene with making some active changes that help clients not just have to escalate into that higher state of threat or higher state of volitional action that makes them more at risk for doing impulsive things that could lead to death.
Katie Vernoy 48:04
Yes. When we, when were talking about hospitalizing someone against their will. And the story that you shared or the statements that you shared, it just reminds me of that feeling when you know, this is the only choice. And I think there’s there’s an inevitability that I feel and maybe I’m talking about it too emotionally. But for me, like there’s that that feeling that you get when it’s like Ooh, there’s no other choice. And only at that point, do I believe hospitalization, especially hospitalization against someone’s will, should be encouraged or should be initiated, I guess is the right word. When we look at the different levels of care, there is the option for someone who is feeling like they can’t keep themselves safe to opt in to hospitalization, they can sign themselves in. And that means they can sign themselves out. There’s a little bit more control over the situation, especially during COVID. I don’t even know if they would be accepted because the hospitals were so full. So I don’t know if this is always an option and may not be an option everywhere. But sometimes that was the step to take for some folks who could see a little bit of hope but could not, didn’t have the resources or the ability to keep themselves safe. And they can always leave, right? So it’s it’s a little bit different. It’s it’s, you know, it just came to my mind when we were talking about this because there is a rupture in the therapeutic relationship. When you are sending your client or facilitating a hospitalization against their will. It can save their lives and like your client said it may be something that they hate absolutely horrible thing but kept him alive and so they’re grateful on the other end of it. But that may not always be the case and so folks that will quickly hospitalize, I think it’s, it’s just such a disservice to our clients, it’s disservice to the therapeutic relationship. It’s traumatic, traumatic for the clients. Theoretically, I mean, I guess some folks like it. But most people do not want to go to the hospital. They don’t want to be held against their will for 72 hours or whatever it ends up being. And so I think it’s something where we have to see it as the absolute last resort. And there is a different feeling of fear versus an event. Fear, oh, my gosh, this liability is going to going to really hurt me to No, this is inevitable, I have to hospitalized to me, there’s two different feelings that I have.
Curt Widhalm 50:40
Not only everything that you just said. But hospitalizing clients who don’t need to be hospitalized is actually more dangerous.
Katie Vernoy 50:50
Yes.
Curt Widhalm 50:52
And the evidence on this is coming from a 2019 study that was published in JAMA, and this tracked a number of people who presented to California emergency departments with deliberate self harm. And they found that those who are hospitalized with self harm without the intention to die, were nearly 57 times higher of having a suicide attempt within the following 12 months.
Katie Vernoy 51:26
Wow.
Curt Widhalm 51:27
People who presented with suicidal ideation, but without the activating steps towards death, were 31.4 times higher than those demographically similar Californians in the year after discharge. Not only that, but the risks of death by unintentional injury was 16 times higher for deliberate harm and 13 times higher for that ideation group. And overdoses were 72% higher in self harm groups and 61%, higher in the ideation groups. And this was exacerbated, especially in men, especially in those over the age of 65, and those in the ages of 10 to 24.
Katie Vernoy 52:14
Okay.
Curt Widhalm 52:15
Surprisingly, one of the resilient factors here is those clients who went to the emergency room who are on Medicaid tended to do better than those in all other paying groups.
Katie Vernoy 52:29
Probably because it was more similar to a regular medical visit. Whereas folks who aren’t used to going to the emergency room and kind of being treated that way, it would be pretty different. And that’s a horrible thing to say. But if it’s more this is what I’m used to versus this is, this is hugely different and, and overwhelming and all of those things I can imagine being part of the effect. But when you’re talking about it, it just really highlights that when someone is hospitalized, or sent to the emergency room for non suicidal self injury or any of those things, we have moved the person in front of us to a problem to solve. They it’s dehumanizing to them. I feel like.
Curt Widhalm 53:22
And that is one of the explanations on this. Another explanation is that without the skills to learn how to work through whatever it is the problem that’s coming up at that time, what clients end up getting trained or shaped into doing is, there will be somebody who catches me and brings me to the emergency room. I just need to act up to a high enough level that somebody will do that. And if those protective factors aren’t there, and that leads to this escalatory type behaviors. But what we want to do is hospitalize clients only as the last resort.
Katie Vernoy 54:06
Yeah.
Curt Widhalm 54:07
And unfortunately, you know, we’re in this weird place in our field where we are talking about suicide a lot better than we have in the past. We’re also at that dangerous point where we know just enough as a field about it to know, okay, we need to talk about it, but we don’t know well enough to talk in depth about it. And it’s this dangerous level of Oh, and I’m, I’m hearing this from a lot of my teenage clients of like, we’re afraid to talk to our our school counselors about even just like thoughts of not wanting to be here because school counselors are escalating everything to hospitalization.
Katie Vernoy 54:46
Oh!
Curt Widhalm 54:46
They’re jumping to the most restrictive levels, you know, those things in that very, you know, active suicidal phase. So we’re at that dangerous level of skill attainment when it comes to intervening here. When really what it is, is, okay, let’s have longer conversations about this. Let’s Yes, let’s incorporate everybody in this and this goes to that E part of the action. That GATE approach is extending the action. Yeah, that it’s not just like, okay, you’ve got your safety plan, I’ll see you next week. This is that increasing the contact with the clients. And you know, modern technology allows for us to do this in a lot better ways than we have in the past. And this, again, comes with the right level of intervention that’s necessary. When I do my bigger CE presentation on this. A lot of people ask me like, well, will you accept, like a text message in response from a client? And I go, if that’s the least intrusive means necessary for that particular client? Yeah, sure.
Katie Vernoy 55:53
Yeah.
Curt Widhalm 55:54
Now, that might be only because I’ve known that client for like, five years, and they’ve got this really good, trustworthy, you know, sort of like, I’m going to reach out and I have a history of reaching out. But if that’s what’s the least intensive thing that I need to do, Yes. If what I need to do is call a client in between every single session and be like, Hey, I have two minutes. I’m thinking of you. I’m checking in on you right now, how are you doing? Did you get a hold of your psychiatrist yet? Do you need me to annoy your psychiatrist on top of this to respond to you? Because post intervention, one of the most resilient things that shows up in the literature, is having a psychiatric appointment, within a week of a suicide attempt is one of the best protective factors for going forward.
Katie Vernoy 56:40
And that means theoretically, medication.
Curt Widhalm 56:44
Yes.
Katie Vernoy 56:44
I mean, is that what we’re we’re saying?
Curt Widhalm 56:46
Yes.
Katie Vernoy 56:47
Okay.
Curt Widhalm 56:50
So extending the action is not just hoping that clients take a good safety plan. And a safety plan is something that identifies what triggers are. It’s something that has specific actions for clients to do when those triggers are presented. Has the list of people that they can call and rely on. And if you’re really doing a good job for your clients, it’s spending some time in session and having them call those people and be like, Hey, I’m going through some stuff right now, I’m not feeling like myself, I am making a list of people that I can rely on to call in these situations. I’m sitting here with my therapist, I’m letting you know that you’re on this list for me. Can you respond to me and like this next week, if like, I’m reaching out to you and really need help? Like, it’s not just listing the people, it’s letting those people know, yeah, I’m going through some shit.
Katie Vernoy 57:45
What it also is something where, as a therapist, if we’re looking at liability, and I know this is a little bit dehumanizing in itself, but as a therapist, I want to know that they actually have access to those folks, they’re not just people that they hope will show up for them. And then not having, you know, having those people deny them is another rejection and another motivational moderator right?
Curt Widhalm 58:10
Yeah.
Katie Vernoy 58:10
And so I think it’s that element of doing that. I, I like this very hands on approach, and I can already hear folks, you know, in my head, you know, in these Facebook groups saying, Well, I don’t have time to do that, like, I, I can’t do that, or that’s too intrusive, or too, you’re working harder than the client, you know, all these things that people get very worried about is like, Okay, well, if I do a good safety plan, I, I’ve done my job. And what you’re saying is no, you need to actually as a human, reach out to this other human and meet them where they are, so that you can continue to help keep them alive until your next appointment.
Curt Widhalm 58:10
Yeah.
Katie Vernoy 58:10
So one of the things I’ve seen in and done and taking responsible action, and extending the action is potentially increasing frequency of sessions. Setting up whether you want to call it coaching calls, a la DBT or check in calls. I think being able to for folks who are worried about this additional time, I think there is ways to structure it, and/or if it’s if this is a concern, get paid for this extra stuff. And so I think it’s something where being able to identify how does this fit into my practice, so that if I have a suicidal client, does it make the most sense for them? Does it make the most sense for me to have an additional session? Does it make the most sense for them to have check in calls or check in texts or check in messages in your portal? Whatever it is, it’s determining how do you set this up so that works for you? Because if you’re not going to consistently do it, you’re not going to remember to do it. If you’re going to feel resentful against your client because they’re taking a lot of extra time that you don’t have because your practice is super full or you take mostly insurance, you have a higher caseload. I think being able to identify how you structure your practice so you can fit these things in and feel good about doing them. Because they are your responsibility. I think that’s important.
Curt Widhalm 1:00:19
I think that if you are making these plans with your first suicidal client, and you’re building your structure around them, as you’re going through it, your failure to plan is planning to fail.
Katie Vernoy 1:00:33
Yes.
Curt Widhalm 1:00:33
And this is where having all of these things in place, upfront, like, once you finish this episode, and you do your CE stuff, then implement this stuff now before you end up with suicidal clients. So that way, it’s less of a shock to you, it’s less scrambling around, it’s something where, yes, it can be an inconvenience to have to check in with clients a little bit more to make sure that they’re following through on their resources. It might take elevating things to beyond you as an individual being the only one responsible for the client. But it’s also really inconvenient for clients to die. And I think that there’s a balance here of like, okay, we’re talking about literal life and death situations here. And, again, I’m going to emphasize, this is for acute stage suicide, this is not the chronically suicidal, the fives and sixes that you’re needing to call 15 times day. This is to get through the very acute phase to make sure that people are staying alive.
Katie Vernoy 1:00:33
Yeah.
Curt Widhalm 1:00:33
And, you know, if it’s something where you need support in your practice to be able to do this. Identify that as your own risk factor as far as being able to work with clients once they reach this state. And you can imagine having a practice that’s working with really high functioning individuals who might present with very few risk factors, but that doesn’t mean that your practice is going to never have somebody who faces suicidality.
Katie Vernoy 1:02:21
Yeah.
Curt Widhalm 1:02:22
And it worth kind of that, you know, ounce of prevention, pound of cure type, you know, statements right here of like, I would rather you, you know, curse me out and be like, Curt, I spent two extra hours putting all of these things in place, and I spent five years and never had a suicidal client. Good job, congratulations, you can be upset with me.
Katie Vernoy 1:02:47
Well, and I want to get really practical, because I think as the Survival Guide, we want to actually say this step. So one of the ways that I have done this is I front load my week with therapy clients, and have the end of the week for second sessions, if I need them. I like to have my free days to do marketing to do long weekends, whatever. And so I build that in where the second half of the week or the second, you know, like Thursday, Friday, I have the availability to do second sessions, reschedules, that kind of stuff, it helps me to keep those clients in there and available. I have built in breaks in my schedule, so I’m not back to back to back to back to back, I have breaks. So I can call people back, I can make sure that I have a little bit of time. And I can truly say and do almost a DBT coaching call, I can say I’ve got 15 minutes. And so I build that in. I think the other piece is making sure that your clients know they can reach out to you. I don’t get a lot of clients needing extra calls. But I tell all of them, if something comes up and you need to talk with me, please reach out and we can schedule a call or an extra session. I offer half sessions, I offer a lot of things to be able to have that, to meet them where they are so that they can get the, the support they need. And so to me, I just wanted to point that out. Because it can be hard if you’ve if you’re locked in to 30 client hours, and you’re back to back and there’s just no extra space and so when a client is in crisis, you are in crisis. I think we don’t want that to be the case. So set up your schedule so that you can do these things. It’s good for having breaks to respond to new client inquiries, to be able to check on clients, for example, and make sure that you implement in a set you know, in your assessment, make sure that you’re assessing for risks, risk factors and protective factors, which we talked about last week. And then make sure that you’re using the Columbia scale, the LRAMP something especially when you’re when your clients are moving into that entrapment phase or active suicidality phase that you can truly understand and assess for risk, and have the steps you need to create a robust safety plan.
Curt Widhalm 1:05:08
Yes.
Katie Vernoy 1:05:09
Okay.
Curt Widhalm 1:05:12
And when I’m totally getting DBT me out of all of this is. And in addition to that, you can have all of the wonderful plans that you have. And there’s going to be times where you also will need to accept that okay, sometimes I have the best plans in the world and things are still, you know, going all all sorts of whackadoo. That a lot of what I do is try and make some times available, you know, for clients or respond back to them. I’m not available right at this moment, here’s my next availability, here’s when I can get back to you on this phone call. And, you know, kind of my philosophy, as far as my practice goes on this is I will respond when it’s most appropriate. You know, and I don’t, I don’t particularly have absolutely hard, you know, I don’t take calls after this time. I don’t take calls before this time. Because sometimes when’s appropriate is going to be whenever it’s appropriate. And there’s and for most clients, this acute phase is going to be a few days, maybe a week, like this is not things where you have to have, and I’m saying that in the if you respond appropriately, you’re going to help clients move out of these feelings very well. But this is not things where you’re going to have you know, this be what you’re doing week after week after week. Make an adjustment for that week to be able to say, Okay, I don’t normally have this time, I’m making this time available because this is extending our contact, this is making things appropriate, these are the things that we can adjust to here. One thing that I do want to talk about here, and this is going to blend into kind of two things. And I am going to emphasize the first one more than the second one. But clients are at the most risk in these transitions, when you are referring to different levels of care. That clients were used to you being their service provider, that it’s during these transition phases that people are not picking up on where the level of crisis actually might be for the client. And one of the core risk management things that you want to do is extending your actions is being able to be in contact with other providers. Now, a lot of times this is going to be to higher levels of care. And if it’s hospitals, then those people that you’re referring to end up not necessarily being available at the same times because they’ve got crises that they’re dealing with all of the time. And this comes to having good documentation that you’re able to send when those clinicians can review it themselves, not necessarily just hoping that magically you’re going to find a time in the 72 hours to make phone contact with each other. So good documentation is an important part of this that helps to outline what your client’s risk factors are, what their motivational factors have been, what their volitional factors have been, and really being able to communicate that because I will share one last story here. One client that I had referred to a local hospital during COVID, you were talking about the difficulties of finding beds, ended up having to be transported to a completely different part of the state. Now I’m used to some of the local hospitals and why I refer to a couple of ones around me is because they’re really good at working as far as with teams and having a good team approach to this. But when this client got sent to a hospital in another part of the state, and I was talking with parents, I’m like, Oh, great. Can I get the caseworker who’s working in the hospital? Can I get their contact information so that way we can start to coordinate aftercare plans and extending the treatment and doing all of my good parts. And so I call up the caseworker and I say, Hey, I’m Curt Widhalm. I’m the therapist who has been working on an outpatient basis, this is what we’re doing and the caseworker goes, hold on, hold on. We don’t do that here. We don’t talk to the outside providers.
Katie Vernoy 1:09:51
Whoa.
Curt Widhalm 1:09:53
And this client was held for 72 hours and it was a, it was a hotel stay for the client that they didn’t really do anything. The discharge for this client was giving him his cell phone back and telling him to call his parents and come and pick him up. And the documentation coming back from the hospital, merely stated, released to the therapist of record, like there was no coordination back to me of anything that happened in the hospital, I have no idea if they did anything at all. And according to this client, they had him watch TV, and they woke them up every couple of hours.
Katie Vernoy 1:10:32
Wow.
Curt Widhalm 1:10:34
So this is something where the lack of communication, the lack of a team approach, the lack of any sort of documentation there, does not do anything for this client, or any of the care people around him to help look at anything that might prevent him from ending up in the same situation in the future. And so this is a plea for good documentation in this because not only is it going to protect you in case there’s any liability factors that come up. But this really helps to show your thought process in intervening with the clients. In a good way, if you miss something, it gives somebody else the opportunity, if they’re working on that documentation in real time with you being like, Oh, we see that this is missed, we need to fill this in. It doesn’t rely on you being able to talk to people on the phone, it’s something that can actively be handed around. And if you do it in a clear way, makes it easy to continue treatment and work as a team there.
Katie Vernoy 1:11:40
I think that’s a great idea. And I think especially if you’re able to get a summary that someone will really take a look at I think it assuming it’s not the hospital you sent your client to during the pandemic, something that people would be really appreciative of. So I think that’s a great idea.
Curt Widhalm 1:11:57
We would love for you to let us know what you think about this episode, follow us on our social media, join our Facebook group, the Modern Therapists Group. If you really liked this long form content, either follow through on the CE stuff, that’s one of the ways that you can support us. You could also be become a patron and get some of the wonderful benefits out of patronizing us?
Katie Vernoy 1:12:22
Over on Patreon.
Curt Widhalm 1:12:23
Over on Patreon, and until next time, I’m Curt Widhalm with Katie Vernoy.
Katie Vernoy 1:12:28
Thanks again to our sponsor, Thrizer.
Curt Widhalm 1:12:31
Thrizer is a new billing platform for therapists that was built on the belief that therapy should be accessible and clinician should earn what they are worth every time you build a client through Thrizer. An insurance claim is automatically generated and sent directly to the clients insurance. From there Thrizer provides concierge support to ensure clients get their reimbursement quickly and directly into their bank account. By eliminating reimbursement by cheque, confusion around benefits and obscurity with reimbursement status they allow your clients to focus on what actually matters rather than worrying about their money. It is very quick and easy to get set up and it works great with EHR systems.
Katie Vernoy 1:13:12
Their team is super helpful and responsive and the founder is actually a longtime therapy client who grew frustrated with his reimbursement times. Thrizer let you become more accessible while remaining in complete control of your practice. Better experience for your clients during therapy means higher retention, money won’t be the reason they quit on therapy. Sign up using bit.ly/moderntherapists and use the code ‘moderntherapists’ if you want to test Thrizer completely risk free, you will get one month of no payment processing fees meaning you earn 100% of your cash rate during that time.
Curt Widhalm 1:13:47
Once again, sign up at bit.ly/moderntherapists and use the code ‘moderntherapists’ if you want to test Thrizer completely risk free. This episode is also brought to you by Simplified SEO Consulting.
Katie Vernoy 1:14:02
These days most people go to Google when they’re looking for a therapist and when they start searching you want to make sure they find you. Simplified SEO Consulting offers a variety of training options to help meet you where you are in your website journey. Led by professionals with a background in education and mental health who truly understand our field the upcoming Cruise is a unique opportunity to learn to optimize your website have time to practice what you learn, and the ability to get feedback from leading SEO professionals in our field.
Curt Widhalm 1:14:31
To reserve your spot before it fills up. Go to simplifiedseoconsulting.com.
Katie Vernoy 1:14:37
Once again go to simplifiedseoconsulting.com to check out all the information on the cruise. Just a quick reminder if you’d like one unit of continuing education for listening to this episode, go to moderntherapistscommunity.com, purchase this course and pass the post test. A CE certificate will appear in your profile once you’ve successfully completed the steps.
Curt Widhalm 1:14:59
Once again that’s moderntherapistscommunity.com
Announcer 1:15:03
Thank you for listening to The Modern Therapist’s Survival Guide. Learn more about who we are and what we do at mtsgpodcast.com. You can also join us on Facebook and Twitter. And please don’t forget to subscribe so you don’t miss any of our episodes.





SPEAK YOUR MIND