Risk Factors for Suicide: What therapists should know when treating teens and adults
Curt and Katie chat about suicide risk factors. Suicide rates have been increasing across the nation and there is an increasing need for the mental health workforce to be prepared to assess and intervene with clients of all ages. We take an in-depth look at the risk and protective factors associated with suicidal ideology and behaviors in both teens and adults. We also lay the beginning foundations of a suicide model to help clinicians better understand and intervene with clients exhibiting suicidal thoughts. This is a continuing education podcourse.
Click here to scroll to the podcast transcript.Transcript
In this podcast episode we explore what makes someone more likely to attempt suicide
We’ve talked frequently about suicide, but thought it would be important, especially during Suicide Prevention Awareness Month, to go more deeply into the risk factors that make someone more likely to attempt and complete suicide.
What are the highest risk factors for suicide?
“Anxiety Sensitivity… the fear of the feelings of being anxious… is even more so correlated with suicidal ideation and suicide attempts than depression is.” – Curt Widhalm, LMFT
- Defining acute, active suicidality (versus passive or chronic suicidality or non-suicidal self-Injury)
- Going beyond the list of risk factors to how big of a risk each factor is for attempting or completing suicide
- Exploring how impactful a previous attempt is on whether someone is likely to attempt of complete suicide
- The importance of getting a complete history of suicidality and suicide attempts at intake
- The impact of family members who have attempted or died by suicide
- Alcohol and other substance use and abuse as an additive risk factor
- Cooccurring mental disorders (eating disorders, psychosis and serious mental illness, depression, anxiety and anxiety sensitivity, personality disorders)
- Child abuse history, especially folks with a history of sexual abuse history
- Life transitions, especially unplanned and sudden life transitions
- Owning a firearm makes you 50 times more likely to die by suicide
- Racial differences in who is more likely to attempt or complete suicide
- Living at a high elevation
What are additional risk factors for suicide specific to teens?
- Early onset of mental illness
- Environmental factors
- Exposure to other suicides (social media, contagion)
- Not being able to identify other options
- Seeking control over their lives and lacking impulse control leading to suicide attempts
- The importance of communication and the potential for a lack of communication
- Bullying and lack of social support, without a way to escape due to social media and cell phones
What are protective factors when assessing for suicidality?
“Just because protective factors are present doesn’t mean that they balance out risk factors [for suicide].”– Curt Widhalm, LMFT
- Reasons for living, responsibility to others
- Spirituality or attending a place of worship that teaches against suicide
- Where you live based on cultural or societal factors
- Having a children or child-rearing responsibilities, intact marriage
- Strong social support, employment
- Relationship with a therapist
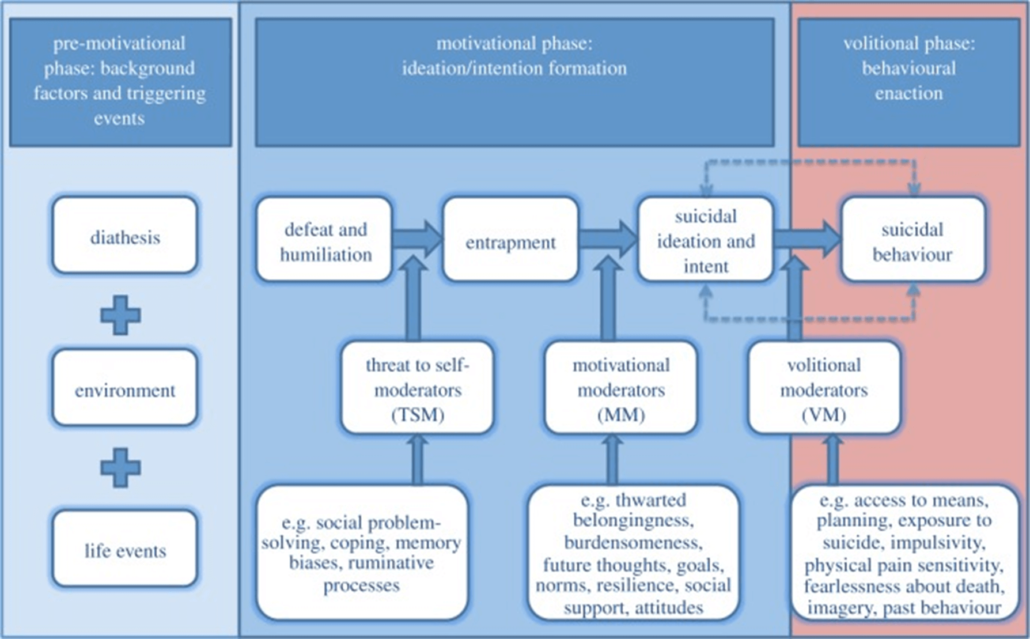
Suicide Model: Integrated Motivational Volitional Model by O’Connor and Kirtley
Our Generous Sponsor for this episode of the Modern Therapist’s Survival Guide:
Thrizer
Thrizer is a new modern billing platform for therapists that was built on the belief that therapy should be accessible AND clinicians should earn what they are worth. Their platform automatically gets clients reimbursed by their insurance after every session. Just by billing your clients through Thrizer, you can potentially save them hundreds every month, with no extra work on your end. Every time you bill a client through Thrizer, an insurance claim is automatically generated and sent directly to the client’s insurance. From there, Thrizer provides concierge support to ensure clients get their reimbursement quickly, directly into their bank account. By eliminating reimbursement by check, confusion around benefits, and obscurity with reimbursement status, they allow your clients to focus on what actually matters rather than worrying about their money. It is very quick to get set up and it works great in completement with EHR systems. Their team is super helpful and responsive, and the founder is actually a long-time therapy client who grew frustrated with his reimbursement times The best part is you don’t need to give up your rate. They charge a standard 3% payment processing fee!
Thrizer lets you become more accessible while remaining in complete control of your practice. A better experience for your clients during therapy means higher retention. Money won’t be the reason they quit on therapy. Sign up using bit.ly/moderntherapists if you want to test Thrizer completely risk free! Sign up for Thrizer with code ‘moderntherapists’ for 1 month of no credit card fees or payment processing fees! That’s right – you will get one month of no payment processing fees, meaning you earn 100% of your cash rate during that time.
Receive Continuing Education for this Episode of the Modern Therapist’s Survival Guide
Hey modern therapists, we’re so excited to offer the opportunity for 1 unit of continuing education for this podcast episode – Therapy Reimagined is bringing you the Modern Therapist Learning Community!
Once you’ve listened to this episode, to get CE credit you just need to go to moderntherapistcommunity.com/podcourse, register for your free profile, purchase this course, pass the post-test, and complete the evaluation! Once that’s all completed – you’ll get a CE certificate in your profile or you can download it for your records. For our current list of CE approvals, check out moderntherapistcommunity.com.
You can find this full course (including handouts and resources) here: https://moderntherapistcommunity.com/courses/risk-factors-for-suicide-what-therapists-should-know-when-treating-teens-and-adults
Continuing Education Approvals:
When we are airing this podcast episode, we have the following CE approval. Please check back as we add other approval bodies: Continuing Education Information
CAMFT CEPA: Therapy Reimagined is approved by the California Association of Marriage and Family Therapists to sponsor continuing education for LMFTs, LPCCs, LCSWs, and LEPs (CAMFT CEPA provider #132270). Therapy Reimagined maintains responsibility for this program and its content. Courses meet the qualifications for the listed hours of continuing education credit for LMFTs, LCSWs, LPCCs, and/or LEPs as required by the California Board of Behavioral Sciences. We are working on additional provider approvals, but solely are able to provide CAMFT CEs at this time. Please check with your licensing body to ensure that they will accept this as an equivalent learning credit.
Resources for Modern Therapists mentioned in this Podcast Episode:
We’ve pulled together resources mentioned in this episode and put together some handy-dandy links. Please note that some of the links below may be affiliate links, so if you purchase after clicking below, we may get a little bit of cash in our pockets. We thank you in advance!
References mentioned in this continuing education podcast:
Bodell, L. P., Cheng, Y., & Wildes, J. E. (2019). Psychological Impairment as a Predictor of Suicide Ideation in Individuals with Anorexia Nervosa. Suicide & life-threatening behavior, 49(2), 520–528. https://doi.org/10.1111/sltb.12459
Borges, G., Bagge, C. L., Cherpitel, C. J., Conner, K. R., Orozco, R., & Rossow, I. (2017). A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychological medicine, 47(5), 949–957. https://doi.org/10.1017/S0033291716002841
Bostwick, C. Pabbati, J. Geske, A. McKean (2016) Suicide Attempt as a Risk Factor for Completed Suicide: Even More Lethal Than We Knew Am. J. Psychiatry, 173 (11), pp. 1094-1100, 10.1176/appi.ajp.2016.15070854
Brådvik, L. Suicide risk and mental disorders. Int. J. Environ. Res. Public Health 2018, 15, 2028
Campisi, S.C., Carducci, B., Akseer, N. et al. (2020) Suicidal behaviours among adolescents from 90 countries: a pooled analysis of the global school-based student health survey. BMC Public Health 20, 1102. https://doi.org/10.1186/s12889-020-09209-z
Doyle, M., While, D., Mok, P.L.H. et al. Suicide risk in primary care patients diagnosed with a personality disorder: a nested case control study. BMC Fam Pract 17, 106 (2016). https://doi.org/10.1186/s12875-016-0479-y
Martin, M.S., Dykxhoorn, J., Afifi, T.O. et al. (2016) Child abuse and the prevalence of suicide attempts among those reporting suicide ideation. Soc Psychiatry Psychiatr Epidemiol 51, 1477–1484. https://doi.org/10.1007/s00127-016-1250-3
O’Connor RC, Kirtley OJ. The integrated motivational-volitional model of suicidal behaviour. Philos Trans R Soc Lond B Biol Sci. 2018;373
Stanley, I. H., Boffa, J. W., Rogers, M. L., Hom, M. A., Albanese, B. J., Chu, C., Capron, D. W., Schmidt, N. B., & Joiner, T. E. (2018). Anxiety sensitivity and suicidal ideation/suicide risk: A meta-analysis. Journal of consulting and clinical psychology, 86(11), 946–960. https://doi.org/10.1037/ccp0000342
Twenge, J. M., Cooper, A. B., Joiner, T. E., Duffy, M. E., & Binau, S. G. (2019, March 14). Age, Period, and Cohort Trends in Mood Disorder Indicators and Suicide-Related Outcomes in a Nationally Representative Dataset, 2005–2017. Journal of Abnormal Psychology. Advance online publication. http://dx.doi.org/10.1037/abn0000410
*The full reference list can be found in the course on our learning platform.
Relevant Episodes of MTSG Podcast:
Rage and Client Self-Harm: An interview with Angela Caldwell
How to Understand and Treat Psychosis: An interview with Maggie Mullen
Navigating the Food and Eating Minefield: An interview with Robyn Goldberg
How Therapists Promote Diet Culture: An interview with Rachel Coleman
Working with Trans Clients: Trans Resilience and Gender Euphoria: An interview with Beck Gee-Cohen
Who we are:
 Curt Widhalm, LMFT
Curt Widhalm, LMFT
Curt Widhalm is in private practice in the Los Angeles area. He is the cofounder of the Therapy Reimagined conference, an Adjunct Professor at Pepperdine University and CSUN, a former Subject Matter Expert for the California Board of Behavioral Sciences, former CFO of the California Association of Marriage and Family Therapists, and a loving husband and father. He is 1/2 great person, 1/2 provocateur, and 1/2 geek, in that order. He dabbles in the dark art of making “dad jokes” and usually has a half-empty cup of coffee somewhere nearby. Learn more at: http://www.curtwidhalm.com
 Katie Vernoy, LMFT
Katie Vernoy, LMFT
Katie Vernoy is a Licensed Marriage and Family Therapist, coach, and consultant supporting leaders, visionaries, executives, and helping professionals to create sustainable careers. Katie, with Curt, has developed workshops and a conference, Therapy Reimagined, to support therapists navigating through the modern challenges of this profession. Katie is also a former President of the California Association of Marriage and Family Therapists. In her spare time, Katie is secretly siphoning off Curt’s youthful energy, so that she can take over the world. Learn more at: http://www.katievernoy.com
A Quick Note:
Our opinions are our own. We are only speaking for ourselves – except when we speak for each other, or over each other. We’re working on it.
Our guests are also only speaking for themselves and have their own opinions. We aren’t trying to take their voice, and no one speaks for us either. Mostly because they don’t want to, but hey.
Stay in Touch with Curt, Katie, and the whole Therapy Reimagined #TherapyMovement:
Consultation services with Curt Widhalm or Katie Vernoy:
Connect with the Modern Therapist Community:
Our Facebook Group – The Modern Therapists Group
Modern Therapist’s Survival Guide Creative Credits:
Voice Over by DW McCann https://www.facebook.com/McCannDW/
Music by Crystal Grooms Mangano https://groomsymusic.com/
Transcript for this episode of the Modern Therapist’s Survival Guide podcast (Autogenerated):
Curt Widhalm 0:00
This episode of The Modern Therapist’s Survival Guide is brought to you by Thrizer.
Katie Vernoy 0:03
Thrizer is a modern billing platform for private pay therapists. Their platform automatically gets clients reimbursed by their insurance after every session. Just by billing your clients through Thrizer you can potentially save them hundreds every month with no extra work on your end. The best part is you don’t have to give up your rates they charge a standard 3% processing fee.
Curt Widhalm 0:24
Listen at the end of the episode for more information on a special offer from Thrizer. Hey, modern therapists, we’re so excited to offer the opportunity for one unit of continuing education for this podcast episode. Once you’ve listened to this episode, to get CE credit, you just need to go to moderntherapistscommunity.com register for your free profile, purchase this course, pass the post test and complete the evaluation. Once that’s all completed, you’ll get a CE certificate in your profile, or you can download it for your records. For a current list of our CE approvals, check out moderntherapistscommunity.com.
Katie Vernoy 1:01
Once again, hop over to moderntherapistscommunity.com For one CE once you’ve listened.
Announcer 1:08
You’re listening to The Modern Therapist’s Survival Guide where therapists live, breathe and practice as human beings. To support you as a whole person and a therapist, here are your hosts, Curt Widhalm, and Katie Vernoy.
Curt Widhalm 1:24
Welcome back modern therapists, this is The Modern Therapist’s Survival Guide. I’m Curt Widhalm, with Katie Vernoy. And this is the podcast for therapists where we talk about the things that happen in our practices, the things that happened in our lives, the things that happened with our clients. And this being Suicide Prevention Awareness Month, we are focusing our CE episode on doing suicide assessments and interventions, we’re gonna make this into a two part episode. So next week, even though it’s no longer Suicide Prevention Month, we’re gonna have a little bit more of a follow up in depth. So follow the directions from the intro and outro, on how you can get your CEs through us. And we appreciate your support in doing that. In our back catalogue of episodes, we’ve covered suicides in a number of episodes, I don’t know, like 17, 18 at this point.
Katie Vernoy 2:25
I think it is 18 at this point, yeah.
Curt Widhalm 2:27
It’s a serious topic. And one that the more that we ended up talking about this, the easier that it becomes to talk with our clients about it. And that’s, you know, one of those things that a lot of developing therapists, you know, kind of really struggle with even just bringing up the word suicide. So, in modeling that it’s okay to talk about this, we should keep talking about it, we are going to embrace that there’s some more in depth stuff that we’ve come across in our studies, our trainings, the trainings that I give, particularly around this, I have a six hour workshop that goes into even more depth in what we’re talking about here over the next couple of weeks. And hopefully, we’ll be able to have that up on our learning platform soon. So as we dive into this first episode, here, we’re going to be focusing a lot more on risk factors, protective factors, getting into kind of the formation of why people become suicidal in the first place. We’re going to talk a little bit about some suicides models as far as how we frame what our understanding of how our clients got there, and what we can start to do about it. We’ll focus our second episode more on the continuation of the assessments and how that leads into interventions and post follow up care.
Katie Vernoy 3:54
So I know that one of the things we’ve talked about is making sure that we also include some things that are specific to teens. I think that’s really important. A lot of our back catalogue is talking about therapists and adults. And I think a lot of the study has been on those folks, not therapists, particularly but adults, especially when we’re reading the news, and we’re identifying that teen suicide seems to be going up. And there’s a lot of mental health concerns, especially coming out of the pandemic and all that’s going on in the world. We wanted to make sure that our modern therapists can do a good job with this stuff, not just with their adult clients, but also with their teens. And as this is an episode on suicide, just a content warning. We’re going to be talking about some stuff that’s pretty heavy. Please take care of yourself. If this isn’t the topic you want to be talking about today. Please come on back to it a different week. But as Curt was saying, I think it’s really important that we do talk about this but just you know, kind of be ready for triggers and different things as we’re talking through suicide and suicide assessment.
Curt Widhalm 5:00
So a couple of definitions here just to start with and frame what we’re talking about. And when we are talking about suicide, we’re talking about an acute deliberate act of self harm undertaken by an individual with at least some intention to die. And we’re making that clear from the very beginning, because there’s a couple of related sort of presentations of clients that we don’t want to get into the weeds about. One of those is people who self harm without the intention to die. And we have a wonderful episode with Angela Caldwell that…
Katie Vernoy 5:41
Oh, yeah, that was such a great episode. Yeah, we’ll definitely put that in the show notes that the non suicidal self injury, I think we call it rage, something, there’s rage in the title, it’s a really, really good episode that also specifically talks about teens as well.
Curt Widhalm 5:56
And we’re also going to talk a little bit about those clients that present with a chronically kind of suicidal sort of presentation, but are not in that acute sort of stage where they are at risk of moving into the acts that cause or follow through on those intentions to have death. So some of the stuff that we’ll talk about fits with that second category there, but we are not addressing that as kind of the primary target of these two episodes here. I know that for a lot of the presentations that I’ve attended, that one of the things that kind of gets glossed over quite a bit, is a lot of presenters will just put up this list of risk factors. Of things that make clients you know, at risk for suicide without really getting into a lot of the finer details of just how much of a risk any of these things are, you know, we’ll hear things like, you know, sudden life changes or things like this that don’t really pay attention to kind of the whys, or how in depth that particular risk factors actually show up. Yeah, and many of us have heard things like the most common predictor of somebody making a suicide attempt is having a previous attempt themselves.
Katie Vernoy 7:26
Yeah.
Curt Widhalm 7:27
And that does continue to hold true that the most potent risk factor is a prior history of suicide attempts, and about half of all deaths by suicide are a follow up attempt to a previous attempt that has happened.
Katie Vernoy 7:41
So I think that’s something that therapists know, but how, how much more likely is it?
Curt Widhalm 7:49
2016 longitudinal study by Bostwick et all talks about ‘Suicide Attempt as a Risk Factor for Completed Suicide.’ That’s the title of it. They looked at nearly 1500 enrollees who they followed after a attempt, and 81 of those about 5% perished on another attempt within 12 months.
Katie Vernoy 8:19
Oh, wow.
Curt Widhalm 8:20
And this is particularly disproportionate towards males that 76.5% by males as compared to 23.5% by females. I will say that a lot of the research that I’ve come across on general suicide studies, unfortunately, looks at genders in the binary. I know that some of the LGBTQ plus stuff that we’ve talked about in a couple of our other episodes that we’ll also link in our show notes are additive risk factors as well. But a lot of the longitudinal research studies have unfortunately only looked at males versus females and don’t really account for a lot of non binary folks in their populations.
Katie Vernoy 9:05
Well, and I think especially for for trans youth, I’ve heard a number of times that for trans teens, the risk of suicide is extremely high. And so we have a couple of episodes that will be specifically on one on trans youth and one on kind of the trans experience that we’ll put in the show notes.
Curt Widhalm 9:24
They went on to say that of those who ended up dying by suicide 72.9% used guns. And compared to all other methods, this is significantly higher. And they found that there were two limitations within their predictions of a suicide risk after a suicide attempt. The first was that subjects had really not been specifically studied from their first lifetime attempt, but rather from first attempts made within the study periods just out of convenience.
Katie Vernoy 10:03
So we don’t know if this is one after the other, and they were successful at their last attempt.
Curt Widhalm 10:10
So this does give credence to what I think a lot of us kind of implicitly know, which is that not only is a previous attempt one of those higher risk factors, but it’s a recent previous attempt that the more distant that something is in the past, while it’s still an indicator of a future likelihood to make an attempt. It’s something where it’s not, you know, just because somebody did something 30 years ago, that they’re immediately at risk for doing something now.
Katie Vernoy 10:40
I think that’s a good point. I think a lot of folks get very scared of this and don’t know how to, to react. And even in thinking about this, I, I’m glad that we’re talking through the risk factors in this way, because I think so many folks will will hear about a previous attempt, or they’ll just hear the words, you know, I don’t want to live or those types of things in a session, and they’ll overreact. And so I think really understanding this risk, these risk factors are really important.
Curt Widhalm 11:10
They go on to say that they found a non fatal one year reattempt, rate of 15%, and a fatal attempt rates of somewhere between 0.5 and 2%. But that 0.5 to 2%, rises to about 5% over the course of nine years. And when we look at the immediacy factor, it’s not just kind of like, once you get past that one year mark, it’s like, okay, the clients good. It’s that yeah, okay, we, we can maybe put 30 years ago, a little bit in the back pocket, but we can’t put seven years ago in the back pocket. That these are things that we want to routinely continue to follow up on. And one of the things that you’ve heard in some of our back episodes, one of the things that I teach in my workshops is that we really should be assessing for suicide in just about every session, whether it’s directly with clients, or indirectly kind of, you know, okay, there’s no presentation of anything that sounds remotely suicidal. But for those clients who have had a previous attempt, it’s not something that, okay, you’ve been my client for like a year and a half now. Your attempt was five years ago. This still pushes to the forefront even more of just how much that we need to continue to ask and check in regularly and directly with our clients, because this additive risk factor does keep continuing to increase.
Katie Vernoy 12:40
Well, I think the other piece with that, and I know, we need to continue on with the risk factors, but I think just taking a little bit of a side trip into this, you know, kind of every session. I think the importance of making it clear to your clients that that topic is on the table is absolutely crucial. And I think that that topic suicide is on the table for every client from the beginning of sessions is important because people are coming to therapy for a reason. I think the thing that that the nuance, I guess that I want to look at is being able to indirectly assess is about understanding the risk factors, and when you need to move from indirect to direct. Because I think some clients, if you ask them every single session, you can get into the humerus like nope, not suicidal today. But I think there’s an element of not seeing the whole person, if that’s the only conversation that you’re having every single session, or if that’s the the primary, that’s where you start every single session. And so I think being able to have that awareness, and really have the open conversation about it, and know when to then go directly into let’s let’s talk through this, what’s going on here. This is sounding familiar, I think is really important.
Curt Widhalm 13:58
And a lot of this starts with your intake paperwork of getting a really serious history of it. And this is the other limitation that was cited in that study is that first lifetime suicide attempts are routinely ignored in case histories as well as in the research. And so that means that it’s systemically underestimated in psychiatric literature about just how often people make attempts. And part of this is getting really good information from our clients. And it oftentimes, you know, slows down the intake process. The more that questions that we have to ask it’s difficult, a lot of clients want to get into whatever it is that they’re seeking out services for. But when we continue to look through a lot of the risk factors here, what we want to be able to do is get a comprehensive history to start understanding just what the risks are when a client does show up in our office. And if we fail to ask the questions from the beginning, it makes it to where it’s even harder to estimate and predict something that we don’t really have good models to be able to predict from.
Katie Vernoy 15:16
That was very, very complex the way you said it. But yes, we do need to ask the question and have the full conversation in the intake.
Curt Widhalm 15:25
Other risk factors, besides a client’s own history of suicide attempts is if an immediate family member has died of suicides, it makes a client about 2.1 times more likely to follow through and die by suicide themselves. So in your intake research intake process, you’re going to want to ask about, you know, has an immediate family member ever attempted and or died by suicide.
Katie Vernoy 15:56
And I think that really should include chosen family and family that they are very close to. I think that families look very different. And so I think being able to really understand who, who is close enough to this individual that that would have an impact.
Curt Widhalm 16:15
We also know about the role of alcohol when it comes to some of these lowering of inhibitions as it comes to, you know, taking really dark thoughts and then adding alcohol into the mix and making it even worse. And this is where it’s not just the presence of alcohol itself, but also the amount of the frequency of use. And alcohol is something that makes it 2.7 to 37 times more likely that a client’s going to follow through on a suicide attempt that results in a death by suicide, but
Katie Vernoy 16:58
37%
Curt Widhalm 17:00
37 times
Katie Vernoy 17:02
37 times. Oh my gosh. So 2 to 37 times more likely to complete suicide if you’re drinking a whole bunch.
Curt Widhalm 17:10
Yes. And that’s from a 2017 study by Borges et all, ‘A meta-analysis of acute use of alcohol and the risk of suicide attempts’ from the Psychological Medicine Journal.
Katie Vernoy 17:22
And we were talking before we were we were recording that’s specific to alcohol, but my understanding is that any kind of substance use probably is worth looking at, for this reason, because of the disinhibition, and, and the, a lot of them actually or have the depressive effects or the, you know, on the opposite end, lots of impulsivity. So not studies there. But I think if you’ve got someone that is having suicidal ideation and using substances, I think it’s worth paying extra attention to it.
Curt Widhalm 17:57
And especially within the context of that definition that we’re working from here of with the intent to die, there are plenty of clients with substance abuse presentations that are engaging in risky behavior due to the substances that is not necessarily with the intention to die. So make sure that you’re separating that out a little bit.
Katie Vernoy 18:22
Yes.
Curt Widhalm 18:25
Next on the list, getting a little bit into the specifics of co-occurring mental disorders, and I’m going to start with talking about anorexia nervosa. And this has a three times percent, excuse me, a three times increase in the risk of dying by suicides. And a lot of our friends in the eating disorder world are very well aware of this. But being able to screen especially for anorexia nervosa, because it is a poor quality of life diagnosis. It’s well documented across a lot of literature that individuals with eating disorders have difficulties in a whole bunch of areas of functioning, psychological, social, physical, work and school, and that the eating disorder behaviors contribute directly to those impairments, which can lead into a lot of feelings of not being able to get out of, you know, the functioning that the eating disorder is causing that they’re then seeing kind of happening around them globally, in a continued negative cycle.
Katie Vernoy 19:34
When you’re talking about that it reminds me of the episode we did with Maggie Mullen. They work with folks with psychosis. And I think there’s this element of disordered or delusional thinking that can come up in a lot of different mental health concerns. And when someone’s mindset is so off from kind of the day to day life, I think that there’s this element of feelings stuck, not being able to make to see any paths to a different direction. And I know we’ll talk about this more when we get into the model. But I think there’s that element of, of when someone is so far down a rabbit hole around their life not being the way they want it to their body not being the way they want it to, I think it can be really hard for them to see out. And so I appreciate this, because I have had clients with eating disorders that either started out suicidal and then went to the eating disorder behavior, or the or the reverse. And I think it’s really important to, to have really clear assessments on those things, because most folks with eating disorders, and we’ll link to the show notes on an episode that we did there, they don’t bring it up in session unless you ask them. I mean, the the harsh self criticism that’s going on inside their head, and the behaviors that they’re doing that really impede their ability to access protective factors, which we’ll also go into. I think it can be a pretty scary space to be in. So I think, glad that we’re talking about this.
Curt Widhalm 21:02
You’re bringing up about serious mental illness about things like schizophrenia and bipolar disorder, Brådvik had a article in 2018 that looked at serious mental illness and suicide risk, and found that things like schizophrenia and bipolar disorder, increase the risk of completing a suicide by 5.8%.
Katie Vernoy 21:23
Oh, my goodness, and that’s pretty high.
Curt Widhalm 21:25
Yeah, moving into more and more risky factors, you know, the one that we often associate with suicidality is depression. And this includes substance abuse induced depression. There was a study out of Australia that looked at the relationship between depression and suicidal behavior. And out of just over 1000 participants, about 1/3 of them reported lifetime depression. And out of that third 48%, reported lifetime suicidal ideation and 16% reported a lifetime suicide attempt. There was a really high correlation between the severity of depression and the risk of making a suicide attempt in both men and women. But the suicide attempts were significantly more common among females with a younger age of depression onset. And this is going to be something when we get into talking about teens a little bit here in a little bit is going to be a continuing factor that I think often gets overlooked. That when we as clinicians start looking at, okay, my client is expressing something about suicide, we tend to focus on just the immediate factors. But we don’t start to get into really the depths of the psychiatric history of when these problems became prevalent in a client’s life. And the logical pathway in looking at this is that the more time that a client has in their life of being able to solve problems without you know, a major depressive episode happening, the more likely they are to have skills already in place that allow for them to deal with difficult situations.
Katie Vernoy 21:25
I think the other piece too, is a lot of us can say like, oh, you know, High School was rough Middle School was rough, you know that life is just hard for teens, right. And yet, I think when we’re really looking at clinical depression in that age bracket, I think it’s really important to recognize, it’s hard to feel hopeful when you’ve not necessarily had a lot of time in your life when you saw hope for the future, or you didn’t feel depressed and your quality of life wasn’t low. And so I think when we can tap into positive memories, and positive times, not only do we have skills and the ability to solve things, solve problems and cope, but we also don’t have a lot of hope, because life has always been this way. And there’s not really any evidence it’s getting any better. You know?
Curt Widhalm 23:29
I think often underestimated in a lot of the workshops or the discussions about suicide that I hear is we focus a lot on depression, we focus a lot on substance use and abuse. What I don’t hear a lot about is how at risk people with anxiety and unfortunately, a lot of the research groups in PTSD with anxiety. And so rather than separating out trauma from anxiety, we get this mix. Researchers do something with that, please.
Katie Vernoy 24:44
Clean that up folks.
Curt Widhalm 24:46
Somebody’s got a PhD project out of that, but not just anxiety, but something called anxiety sensitivity seems to be the biggest risk factor. Have you ever heard of anxiety sensitivity? Or do you know what it is?
Katie Vernoy 25:06
I don’t think I’ve heard of it. But it seems like it’s something that would be kind of the person’s experience with anxiety and their difficulty coping with the feelings of anxiety. Am I Am I on it? Am I close?
Curt Widhalm 25:19
You’re pretty close. Anxiety sensitivity is defined as the extent to which an individual fears, anxiety related sensations.
Katie Vernoy 25:28
Oh, yeah, no, I have a lot of clients who have anxiety sensitivity, then, oh, my goodness, that’s a great way to describe it. I love that.
Curt Widhalm 25:36
So it’s a a fear of the feelings of being anxious. And so as we get into the model, we’ll come back to this point a little bit. But if you’re just afraid of even being afraid of things, it really becomes isolating. And when we talk about, you know, the importance of, you know, protective factors. Of going out, and being able to have good, strong social networks and this kind of stuff. But if there’s this fear of something going wrong, or a social anxiety that’s added to this, this sensitivity is even more so correlated with suicidal ideation and suicide attempts than even depression is.
Katie Vernoy 26:19
Oh, wow, that makes a lot of sense. Because I think to me, I, you know, in hearing this experience of this fear of being anxious, or just this discomfort, and how painful it is to be anxious, and some of my clients feel like there’s no way out, like, they’re just going to always feel this way. It’s, it’s so uncomfortable. And there’s, there’s a lot of emotional dysregulation with no real way of self soothing, that it is terrifying for them.
Curt Widhalm 26:51
Well, and it’s terrifying because it’s a feeling of a loss of control, in addition to whatever else is going on. And, and the meta analysis that was done on this by Stanley et all 2018 ‘Anxiety sensitivity and suicidal ideation/suicide risk: A meta-analysis’ in the Journal of consulting and clinical psychology. They talk about how this just loss of control that leads to greater experiences of of distress, which is kind of a volitional factor when it comes to greater suicide risk.
Katie Vernoy 27:20
Distress is what you’re talking about here.
Curt Widhalm 27:29
Yeah. And especially when they add, you know, any other sort of, you know, co occurring pathologies. If there’s anxiety and depression, anxiety and substance abuse, we’re now looking at greater and greater risks of, you know, any of these feelings, you know, being isolated poses great risks, but when you start adding comorbidities on top of them, it gets even higher. And just something where, again, I don’t see a lot of people talking about anxiety as a really major flag to look for in clients when it comes to suicidal ideation.
Katie Vernoy 28:06
Yeah, I think I think you’re right, I don’t think I’ve heard that either. And to me, it makes so much sense with the extreme, huge emotions and with anxiety and I mean, the anxiety is activating. Whereas if you’re really deep in depression, I mean, maybe these numbers are wrong, so correct me if I’m wrong, but I’ve heard that like, when you’re super far down into depression, you don’t have the wherewithal to complete suicide or to attempt suicide. Whereas with anxiety, you got all the energy you need. And so to me, it seems like there’s a real miss there if people aren’t talking about and assessing their anxious clients for suicidal ideation and and potential suicide attempts.
Curt Widhalm 28:50
Now, our biggest risk factors as far as co-occurring mental disorders comes out of personality disorders, and personality disorders as a whole show a 20 fold increase in suicide risk for patients.
Katie Vernoy 29:04
20 fold.
Curt Widhalm 29:06
Yes.
Katie Vernoy 29:07
Wow. Okay.
Curt Widhalm 29:10
When we isolate out borderline personality disorder, that 20 fold increase goes to 37 times more likely. And when we go to borderline personality disorder with alcohol misuse, we’re at 45 times more likely.
Katie Vernoy 29:24
Okay.
Curt Widhalm 29:25
And these risks tend to follow some of the ways that the diagnostics fall, relative risks are higher for females in this group, and elevated with younger age ranges, especially with earlier onset of diagnostics, particularly closer to 16 years olds but showing a high risk through age 39.
Katie Vernoy 29:49
So diagnosed being diagnosed with borderline personality disorder as female is and especially if they’re also substance use on board or misuse? Almost 50/50?
Curt Widhalm 30:04
Yeah.
Katie Vernoy 30:06
I think that’s, that’s incredibly scary.
Curt Widhalm 30:10
Risk factors also include history of child abuse, Martin et all in a 2016 study ‘Child abuse and the prevalence of suicide attempts among those reporting suicide ideation’ looked at number of participants over the course of 12 months, and out of those who reported suicidal ideation in the past 12 months in the study, 61.2% reported high rates of child abuse. They were 2.56 times more likely to have a suicide attempt than a control group. And for those who had a history of sexual abuse, it was seven times higher than the control group.
Katie Vernoy 30:53
Are these risk factors additive? Do you think? Or is it something where the most prevalent diagnostic or life experience kind of put them in those categories? Because it seems to me like I’m thinking about someone who potentially has borderline personality disorder, an eating disorder, as well as, you know, past childhood trauma and substance abuse? And I feel like, are we, you know, where are we at with that? Because it seems like there’s so many factors that oftentimes are comorbid.
Curt Widhalm 31:25
If I’m completely honest, even with a lot of the meta analyses that I’m reading, is, there’s some understandings of the additive factors of them. That, you know, what we were just referencing with borderline personality and alcohol misuse, that they definitely do show some additive factors. But, you know, hopefully, there’s not somebody who meets all of these risk factors out there, that poor person, if that person does exist, that has all of these diagnostics has all of these other risk factors in place, but it very easily stands to reason that yeah, these things are quite additive, much like ACEs becomes kind of an additive sort of things that all of these risk factors. While the research isn’t like yes, we have definitive proof, I think we have a common understanding that yes, these things definitely show it.
Katie Vernoy 32:22
And for folks who don’t know what ACE, the ACEs study is, it’s a Adverse Childhood Experiences Study that that Vincent Felitti did through Kaiser, I actually include the ACE exam, I guess, or the ACE study questionnaire, in my intakes, it’s actually really helpful.
Curt Widhalm 32:43
Others things that get talked about a lot, and we’re not going to do a deep dive into these we’re going to continue on with our episode here a little bit. But anything that is a sudden change in a client’s life becomes another factor that ends up becoming a multiplier of a client’s risk. And we’re talking about things here, like a sudden loss of employment, a divorce or a separation, somebody runs into legal difficulties, or a very rapid social isolation. These things all serve as motivational factors that are in addition to the risks that somebody may already have as their primary presentation as they show up and become pretty significantly things that we need to address and assess for in our sessions with clients when they are bringing these things up in their sessions with us.
Katie Vernoy 33:42
And I think that really means that a lot of therapists who say they work with life transitions, quote, unquote, really need to understand suicide, even if they don’t typically have more intense cases or, or more severe diagnostics coming into their office. Life transitions is a risk factor for suicide, right? I mean, people are like, Oh, I work with life transitions is like this is a part of life transitions, right?
Curt Widhalm 34:09
Yeah. And, you know, there’s the really nice and stable life transitions of I’m thinking about a career change. And if the right job opens up, then oh, I’ll interview for it and I’ll take it. Those are the plant life transitions, but unplanned ones, and this goes back to talking about trauma here, is there’s oftentimes that need for a sense of control after a trauma, where people will make major life transitions just to get out of some of those anxiety or ruminating feelings. And that ends up becoming something where, if that can also subsequently mean like, your social support system, you know, your work buddies are completely changing. That puts you at a greater risk for not having some of the wonderful protective factors that are in place.
Katie Vernoy 34:58
I think it’s, it’s, it’s something where the more we talk about this, and we’ve had 18 episodes that at least have something involved with suicide in them, I just realized that there’s, there’s no, there’s no one thing that says, Okay, I’ve been able to completely avoid having suicidality show up in my office. Because life can change so quickly things can happen that come out of the blue. And if someone’s coming to therapy, unless it really is solely personal growth, and even then I would argue that things can change in that regard, too. There is some sort of underlying mental health concern that they’re bringing forward. And so much of this stuff, especially with traumas, and sudden life changes, like everyone should be assessing for this. Because even when you and I were talking about preparing for this episode, I was like, Well, you know, I did a lot of this when I was working in other venues. But in my private practice, I work with executives, like many of them are fine, but then I was like, no, no, you know, executives die by suicide, too. And so I think it’s that that piece of really being able to understand what the risk factors are, is important. Do we have more risk factors? Are we moving into protective factors? What are we doing right now?
Curt Widhalm 36:14
Well, this is the part where you had previewed, talking a little bit more about teenagers as well.
Katie Vernoy 36:20
Ah, yes. Okay. So let me just finish this one thing, and then we’ll, we’ll get through it. But I think when we get to protective factors, I think we have these risk factors. But another risk factor is a lack of protective factors. So, when we’re looking through all of this, I think it’s really important to understand the whole picture, because there’s oftentimes, so much that can go into something that may surprise you if you’re not really picking up all of these risk factors.
Curt Widhalm 36:50
So, as I’ve talked about, on the show quite a bit, a lot of my practice focuses on working with teenagers. And a lot of what is readily available, as far as research seems to start to acknowledge here in 2022, that a lot of previous research on teen suicidal ideation and suicide attempts, seems to be researchers and clinicians who are treating teenagers as miniature versions of adults. And don’t look at necessarily the specific factors that go along with being a teenager that stand in addition to the risk factors of adults. But you’ve heard me mentioned a couple of times the earlier onset of a mental illness makes a bigger risk factor. And this can come from a variety of things such as lesser family support, the greater impacts of things like poverty. But the two that I tend to go above and beyond even what a lot of the gold standard protocols for looking at suicidal ideation within teenage clients is, number one, the exposure to other suicides, whether it’s…
Katie Vernoy 38:13
So the kind of social media, families, whatever…
Curt Widhalm 38:16
contagion sort of…
Katie Vernoy 38:17
The contagion sort of stuff, yeah.
Curt Widhalm 38:19
And teenagers pose a lot higher risk of seeing this as an option when somebody does die by suicide. Because in that underdeveloped adolescent brain, the prefrontal cortex is still there…
Katie Vernoy 38:36
Still growing…
Curt Widhalm 38:37
Still growing, still not there. And it really becomes evident when there becomes this hyper focus on trying to get out of the problem. When a teenager interprets another student at school, somebody in the media, somebody on social media who has died by suicide, that that becomes one of the few options that a teenager starts to look at. And when we get into talking about kind of the model of how we look at suicidality, that lack of being able to see other options ends up becoming the biggest kind of conglomerate risk factor from going from ideation into action.
Katie Vernoy 39:25
It seems like with teens that are frequently engaged with their phones, through social media or other types of platforms where they can see a lot and they can see far and it’s an a dissociative act even, kind of scrolling through and watching video after video or whatever it is. It seems like the autonomy of a teenager has diminished in some ways, where they’re either very enthralled to their phone and what everybody is doing. And so they don’t leave their social life at school anymore. They bring their social life with them in their pocket. And then they oftentimes don’t have autonomy in their family life. I mean, when you’re talking about a lot of these things are about trying to take control, I just feel like teens have a lot less control now than they than they had when I was growing up. I know joking that, you know, the Gen X or latchkey kids that watch themselves but like, I think that there’s this element of huge amounts of stimulation and emotional content being fed, where they are also not having control over how they, you know, make how they live their lives.
Curt Widhalm 40:45
And this comes to the other factor that I tend to focus a lot more on when it comes to the teenage population is the role of impulsivity. That well, there are certain personality characteristics and adults that can lead to impulsive behavior. And it may be related to one of the diagnostics that we mentioned earlier. But it may just be personality traits that lead to doing impulsive things that we don’t necessarily think of adolescents on a good day as being really predictable and rational beings.
Katie Vernoy 41:22
With slow deliberate actions that they take.
Curt Widhalm 41:26
Really well thought out cause and effect sort of plans. That especially those teenagers who are presenting as having more impulsive behaviors already, whether it’s part of a diagnostic or not, that when suicidal ideation is present, those are clients that we need to focus on more and have stronger safety planning around. Because of that lack of ability, that lack of ability to have that cause and effect sort of action really play out.
Katie Vernoy 42:01
Well, and to me, you know, and then this is for any kind of clients who’ve come into my office and kind of all of the different times I’ve engaged with treatment around teens. And it just seems like there’s also a lack of communication. And so these factors are even more intense, and the teen is potentially less likely to talk to us about it. So it’s even harder to assess, and really get to the crux of the matter if we’re not able to really dig in and understand the isolation or if we’re not following all of the things on social media and the news and that kind of stuff and knowing if there’s a potential for contagion, or we’re not necessarily seeing the impulsive decisions that a teen is making, because they are, they have put them pulled themselves together before they walk into our office. And so I think it’s something where getting a full picture of what’s happening in the teen’s life, including their relationships with their family members, and how likely they are to bring forward concerns, I think is critical because many teens don’t even want to be in the therapy room with us, at least at the very beginning. And so if we don’t have that, that engagement and that buy in, so much of this is really hard to assess if the caregivers don’t have a sense of what’s going on in their teens life.
Curt Widhalm 43:29
Furthering some of the ideas around, you know, earlier onset of risk factors being present. One of the more robust meta analyses that I’ve seen in looking at teenagers is by Campisi et all, is from 2020 Suicidal behaviours among adolescents from 90 countries: a pooled analysis of the global school-based student health survey, this is in BMC Public Health, looked at teenagers being in two distinct groups. A younger group of 13 to 15 year olds and a older group of 16 to 18 year olds, and they controlled for a phenomenal amount of co-variables here looking at, you know, income disparities, and found that while, that does have some backgrounds contributions to it, that more specifically, the things of looking at within teenagers are again, that social isolation or lack of having friends, as well as things like bullying, and when those things are in place, so there’s a bullying episode that will be coming out here in the next couple of months with but looking at the lack of friends, in addition to the targeted bullying that can happen. And as you just pointed out, where, you know, Gen Xers and a lot of millennials grew up at least being able to go home and kind of, you know, not have to be constantly on social media and be constantly faced with, you know, threatening or, you know, demeaning language or isolation, exclusion. These all become risk factors that particularly affects that younger age group 13 to 15 year olds.
Katie Vernoy 43:35
Sure.
Curt Widhalm 43:37
Particularly 13 to 15 year old females.
Katie Vernoy 45:29
Got it.
Curt Widhalm 45:30
Now, the two groups do end up making it a little bit more balanced when they reach to that 16 to 18 year olds pool. But that’s not necessarily the, you know, everything gets magically better when you turn 16 it’s more of…
Katie Vernoy 45:50
A lot of things don’t get magically better when you turn 16.
Curt Widhalm 45:53
It’s even riskier to be a 13 to 15 year old girl is kind of the takeaway from that.
Katie Vernoy 45:58
Got it. Got it. Yeah, I think there’s, there’s just so much that can be going on in these teenagers lives. And honestly, it’s one of the reasons that I have strayed away from doing that a little bit because I think I, I recognize that you need to have energy and focus and really be able to understand what they’re faced with.
Curt Widhalm 46:24
And a couple of other risk factors that I’ll mention real briefly before we move over to the protective factors, but owning a firearm is one of the highest risk factors that you know, the those exercising those second amendment rights makes somebody a 50 fold times more likely to die by suicide, just by purchasing and owning a firearm.
Katie Vernoy 46:49
So 50 times more likely, okay, this episode’s gonna be banned by the NRA.
Curt Widhalm 46:56
Yep.
Katie Vernoy 46:59
We can decide if you want to keep that in or not correct.
Curt Widhalm 47:04
And there are two particular ethnic groups within the United States that show a higher risk of attempting and completing suicide. Those are white people and American Indians and Alaska Natives.
Katie Vernoy 47:21
Oh, interesting. What do you think that’s about?
Curt Widhalm 47:24
What I’ve seen about Native populations within America is that a lot of the risk factors that we see: poverty, high substance abuse, lack of, you know, a lot of resources, the inability to really move in and out of the communities with continued support from the social structures that are there all pose really big risk factors.
Katie Vernoy 47:52
Makes sense. How about for white people?
Curt Widhalm 47:55
A lot of the research seems to suggest that white people don’t have as strong of ties to family of origins, to communities where they grow up in and tend to isolate more, and tend to cope with things like substances and buying guns. And…
Katie Vernoy 48:14
So rugged individualism may not be as good for our mental health as we thought.
Curt Widhalm 48:22
Now, I’m not going to spend a lot of time on this.
Katie Vernoy 48:25
Sure.
Curt Widhalm 48:26
But one of the greatest factors worldwide that has been shown to be a risk factor for people at risk of suicidal ideation and dying by suicide, is living at elevations above 6000 feet.
Katie Vernoy 48:43
Wow. Okay.
Curt Widhalm 48:45
And there seems to be really strong, you know, consensus that there’s something to this, and it seems to be something that people haven’t quite been able to put, you know, a here’s, you know, an absolute factor. This is true in the United States, it’s true in the Himalayas, it’s true in mountain regions all across the world. So this is not just something where it’s attributable to, you know, just the isolated living of being up on a mountaintop someplace, and, you know, the American west or something where there’s other factors like, you know, higher rates of gun ownership. But across cultures, even in some of the more populated areas within these regions, there seems to be something about the thin mountain air that seems to affect the way that people problem solve when they are feeling stuck in their problems.
Katie Vernoy 49:42
Hmm. So you said you weren’t going to spend much time on it. So where are we going next?
Curt Widhalm 49:51
All right. So we have spent a lot of time talking about risk factors. You brought up some protective factors earlier and I will lead off this section by saying, just because protective factors are present doesn’t mean that they balance out risk factors. There’s no magic formula of, you know, you have four protective factors and two risk factors. So, the pros list outweighs the cons list here.
Katie Vernoy 50:17
I think that’s a good point. Because I, for me, oftentimes, if I’m doing more of an indirect assessment, I do look, you hear more about protective factors, oftentimes, or at least I’m looking for, I’m looking for a future orientation, or a social support network, or reasons to live. Stuff like that. And so I think knowing that some of these risk factors can completely outweigh all of the protective factors, I think it’s important to pay attention to.
Curt Widhalm 50:44
And so the most robust protective factors tend to be reasons for living. Having some sort of, you know, plans for the future that really allows her clients to demonstrate that, hey, I’ve got reasons to live, I really want to get out of this particular situation, but I’m still planning on being there for grandma’s 100th birthday, or, you know, some sort of other future plan that helps to get out of the immediate crisis of that acute suicidal phase.
Katie Vernoy 51:18
Well, and even reason, reasons for living, oftentimes, I know that there’s also a social support one, but it can also be the people who are relying on you, or it can be the animals that your pets or your you know, your friends, or there’s something where you feel tied to some responsibility or some positive thing that even though you can’t access it completely, you still have, you know, a tie to it.
Curt Widhalm 51:45
Right.
Katie Vernoy 51:46
Yeah.
Curt Widhalm 51:47
And that also includes, protective factors also includes things like being free from substances. We mentioned just how risky substances are. But so the inverse holds true. Attending a place of worship or some place of internalized spiritual teachings against suicides and, you know, as Katie and I being based out of California, California shows one of the lowest overall suicide rates within the country. And a lot of the states that show the highest risk of suicides end up being places, particularly in the American West, Montana, Idaho, Wyoming, Colorado, Utah, Nevada, New Mexico, these are all places that, you know, are outside of, you know, a couple of major metropolitan areas, a lot of rural living a lot of high gun ownership places. And a lot of the rates by per 100,000 people who die this is from 2018, data from the CDC, would suggest that Texas would have really high suicide rates, but Texas tends to fall on the lower side of suicide rates.
Katie Vernoy 53:00
Good job, Texas.
Curt Widhalm 53:02
And a lot of this seems to be based on the also strong culture of belonging to religious institutions that a lot of Texans have. The presence in the home of having a child or having child rearing responsibilities. It’s not as significant factor for single men, but men who are married or cohabitating, where there’s children present, this tends to be a pretty strong protective factor. But it’s a lot stronger protector factor in women. And women tend to show more resilience towards suicidal ideation with the greater number of children that they have. And, you know, this isn’t ridiculous, like, women with three or more children kind of tend to taper out as far as how much protective factor it is. So it’s not like go and encourage your clients to have like, bunches of babies just to get through being through suicidal. But the more children that they have to live there for and to, to provide for tends to be a very significant factor for women. Having an intact marriage tends to help men a lot more, they’re two times less likely to make a suicide attempt and complete suicides if they have a intact marriage. Strong social supports, being employed, having a trait of kind of looking towards the positive side of life and having a trusted relationship with a counselor, a physician or other mental or physical health service provider all tend to be really good strong factors.
Katie Vernoy 54:49
That’s us.
Curt Widhalm 54:50
That’s us.
Katie Vernoy 54:51
We’re a protective factor. That’s that feels really positive. So a lot of those things make sense. So I think a lot of those things are protective not just for suicide suicidality, it’s also protective for mental health in general. And so to me, you know, when we’re really looking at assessment and looking at protective factors, it’s all it’s all of the same piece. It’s not like you do a whole assessment that solely for suicide, and then you go and do the rest of the assessment. I mean, this is really a full assessment of what the client has going for them.
Curt Widhalm 55:31
Yes, to kind of wrap up this episodes and lead into next week’s episodes. Next week, again, is we’re going to talk about kind of what to do in your assessments and how to follow up. We’ve been talking about this model a little bit throughout this episode, I want to spend the last little bit here talking about how all of this kind of comes together. And the model that I really like and work from is called the Integrated Motivational Volitional model or the IMV model. And this was developed by Rory O’Connor and further updated by O’Connor and Kirtley. And this looks at there’s three phases when it comes to suicidal ideation and attempts. I will put a graphic that comes from this model into the shownotes. So that way, you can reference this because I think it makes a lot more sense and it’s a lot more tangible when you can see, it’s not just hearing us talk about it on the podcast here. But in this model, the pre-motivational phase is looking at three factors. A lot of us have heard of things like the stress diathesis model, and…
Katie Vernoy 56:56
I always heard of it add it as the diathesis stress model. Interesting.
Curt Widhalm 57:00
Tomato. Oh, O-mot-tots, I guess?
Katie Vernoy 57:10
Toh-mah-tohts.
Curt Widhalm 57:11
But anyway, the diathesis is kind of the personal factors that exist for a client and their, you know, outlook on life, their abilities to handle things, some of their particular diagnostics, the SES class that they’re in, all of those things are individual factors.
Katie Vernoy 57:33
Yes.
Curt Widhalm 57:34
Coupled with the environment that they are living in. And just as an example of this, we’re talking about those teenagers who are in an environment where they’re subject to a lot of bullying, and they also have some sort of news in their life about somebody that they like dying by suicide. These are environmental factors that exist, in addition to those individual factors, as explained by the diathesis.
Katie Vernoy 58:03
Sure.
Curt Widhalm 58:04
And you add to that any sort of life events, you know, a sudden move, a sudden change in, you know, socioeconomic status or loss of a job. These are all pre motivational factors that we need to be prepared for.
Katie Vernoy 58:22
Yes.
Curt Widhalm 58:22
Now, the particulars of somebody’s diathesis, the coping skills that they have, these are things that I believe that can be changed through good mental health work, mental health awareness. It’s when the combination of the diathesis the environment, and the life events are coupled with something called defeat and humiliation. That becomes a threat to the person’s self. This is, you know, the expansion of social problems that really end up making somebody feel like, I can’t get out of this. And it leads to a particular feeling within this model called entrapment. Now, that entrapment really is this feeling that we’ve been referring to all episode of, I can’t get out of this.
Katie Vernoy 58:59
I can’t see another way. I can’t see any way to solve this. I’m stuck.
Curt Widhalm 59:21
And not only can I not see it, I can’t hear other alternatives from the people around me.
Katie Vernoy 59:29
Yeah.
Curt Widhalm 59:30
And this is the particular phase of suicidal ideation that puts people most at risk from going from that: I don’t want to be here. I’m thinking about, you know, suicide, I’m thinking about what life might be like without me or how I just don’t want to have to solve these problems into a more activated phase of I’m thinking about ways to kill myself.
Katie Vernoy 59:58
Yeah.
Curt Widhalm 59:59
And this is is the particular window where we have to intervene in the best way possible for clients that meets their specific needs, that starts to give them a sense of the problems have a way out of them. And we’ll talk a lot more in the next episode of the risks of intervening incorrectly, especially at this stage.
Katie Vernoy 1:00:24
Sure.
Curt Widhalm 1:00:25
But this feeling of entrapment ends up showing up as really ruminative flooding. That they lose the cognitive control to control what their thoughts are. All that they can think about is how stuck that they are. It’s also in this really hyper aroused panic dissociation. And this is often presenting a somatic symptoms that are very panic like and are very unfamiliar for a lot of clients, that when we talked about the risk factors of anxiety earlier, and just especially for those who are anxiety sensitive, that this ends up heightening this entrapment feeling of not only can I not get out of whatever this problem is that’s causing it, I’m experiencing all of these new and unwanted situations here.
Katie Vernoy 1:01:16
Well, and just the way you’re describing it, your mind is going and going and going and you can’t control it, you’re physically feeling overwhelmed, and like something is wrong. To me that feels excruciating, I would imagine that sensation, and that internal experience would be really overwhelming.
Curt Widhalm 1:01:35
And what that ends up doing is it ends up mediating a fear of dying, it gets rid of that cognitive fear of no longer existing, which moves people from that latent suicidal ideation into active suicidal ideation.
Katie Vernoy 1:01:51
And I know you didn’t mention this one, but I saw it on one of the assessment tools that we’re going to talk about in the next episode. But fear of dying actually is a protective factor. So if you if you lose that in this entrapment phase, that really pushes across the finish line, and some for some folks to actual attempts.
Curt Widhalm 1:02:12
And these ultimately lead to what the entrapment definition includes emotional pain, this is that intense negative affect. And this ends up being feelings of guilt, shame, hopelessness, disgrace, rage, and defeat. And that overpowers those essential needs of love, of control, of protecting one’s self image, voiding shame, voiding humiliation, and this is ultimately going to end up in a feeling of desperation.
Katie Vernoy 1:02:47
Which we don’t want our clients to feel this feeling of desperation, if we can help them avoid that.
Curt Widhalm 1:02:55
Out of this episode, we are really hoping that what you’re walking away from is the specific risk factors that really end up contributing and just how rapidly those risk factors can deteriorate into this entrapment phase of the IMV model. And why it’s so important for you to have kind of a global understanding of who your client is, before they ever get to this phase. And, you know, we can have really wonderful nice clients show up. But when those life events end up happening that end up triggering them, if we don’t understand just how sensitive clients are going to be to some of these risk factors, when they’re in that heightened state, it really gives us a better idea to develop a safety plan, which we’ll get into in our next episode of being able to point out here are very, very specific risk factors to you, you know, coming from my teenage practice is you’ve got a test coming up next week. And I know that when you get really anxious about things, that it heightens all of these other feelings, and we’re concerned about how you’re going to be able to cope at that particular time, that helps us to better be able to safely plan with our clients.
Katie Vernoy 1:04:16
And I think the other piece that popped into my head while you were talking is a lot of folks come to therapy in this heightened state, like that’s what, you know, someone’s dragging them into therapy because they see this entrapment or they see this, or they’ve had an attempt or there’s something that’s going on. And so to me, I think the converse is true. Helping someone get that resolved, where they’re able to de-escalate some of these feelings are able to to get to a place where they can actually see hope or see some sort of future those types of things if we can move them out of entrapment, which I’m sure we’ll talk about next time. We may identify new protective factors. We may better under Stand risk factors because in that state of entrapment, we’re not seeing the whole client. We’re seeing that client in a in a space that doesn’t, that maybe some of these protective factors have become less relevant and may not be reported upon. So it also means that we need to be assessing these things over time. Because these things go up and down. The protective factors aren’t still static, the risk factors aren’t static, like, these are things that we need to be paying attention to. And I think, you know, when I look at times when, you know, kind of, I’ve gotten complacent, I’ll say it for myself, like oftentimes, the, what we talk about in therapy is what’s happening this week, which is relevant to some of this stuff, but we’re not necessarily, you know, when I say, Hey, how’s the week going? If someone doesn’t present and doesn’t share some of these things, or does it as a doorknob confession, it’s something that we’re just not getting that information. And so I think we have to be a little bit more direct, a little bit more strategic with asking these questions so that we don’t miss these types of pieces. Because I don’t know how many times this has happened to you, Curt. But like, there have been times when I’ll ask a question based on what I know about a client, I’ll be like, Hey, have you been drinking water? And they’re like, Oh, no, that’s why I’m feeling a lot more depressed right now. You know, it’s like, it’s one of those things where it’s, it’s, it’s being able to know your client well enough to really see what’s going to be coming down the pike for them, and understand the impacts those things typically have, and also on a broader scale, what some of these risk factors can do to clients even when they’ve never shown up before. So I’m excited to continue this conversation, I know we’re going to talk about some tools, assessment tools, as well as and the way you’ve described it as the next one is actually about intervention and planning. It’s just the the assessment, the actual act of doing these assessments is the first stage of safety planning, because it is so, it’s just so entwined. And so I’m looking forward to next week’s conversation, because I think it’ll be very practical. This was very eye opening. This was a lot of data, a lot of a lot of data, a lot of information to take in to say, Okay, what actually could make a difference? And then the next time is very practical. How do you use that information to understand your client, and walk through the phases of getting to a safety plan and intervention and moving through and to follow up and, and how you move forward when someone’s gotten to this acute state. So I’m here for it.
Curt Widhalm 1:07:40
You can find our references and our show notes over at mtsgpodcast.com. And make sure that you follow us on our social media, subscribe if you are not already subscribed. And check out our Facebook group, the Modern Therapists Group. And if you like our long form content, please also consider being a patron and that helps us.
Katie Vernoy 1:08:04
and yeah, and with the Patreon patrons if we do have options so that you can do Q&As with us and you can dig in with us in person over Zoom. To talk about some of these things and ask questions. It’s, it’s a, it’s an offer that we have for our patrons that we would love to share with you.
Curt Widhalm 1:08:22
And make sure that you follow the directions on how to get CEs and until next time, I’m Curt Widhalm with Katie Vernoy.
Katie Vernoy 1:08:28
Thanks again to our sponsor, Thrizer.
Curt Widhalm 1:08:31
Thrizer is a new billing platform for therapists that was built on the belief that therapy should be accessible and clinicians should earn what they are worth. Every time you bill a client through Thrizer an insurance claim is automatically generated and sent directly to the clients insurance. From there Thrizer provides concierge support to ensure clients get their reimbursement quickly and directly into their bank account. By eliminating reimbursement by cheque, confusion around benefits and obscurity with reimbursement status they allow your clients to focus on what actually matters rather than worrying about their money. It is very quick and easy to get set up and it works great with EHR systems.
Katie Vernoy 1:09:12
Their team is super helpful and responsive and the founder is actually a longtime therapy client who grew frustrated with his reimbursement times. Thrizer lets you become more accessible while remaining in complete control of your practice. Better experience for your clients during therapy means higher retention. Money won’t be the reason they quit on therapy. Sign up using bit.ly/moderntherapists and use the code ‘moderntherapists’ if you want to test Thrizer completely risk free, you will get one month of no payment processing fees meaning you will earn 100% of your cash rate during that time.
Curt Widhalm 1:09:47
Once again, sign up at bit.ly/moderntherapists and use the code ‘moderntherapists’ if you want to test Thrizer completely risk free.
Katie Vernoy 1:09:56
Just a quick reminder if you’d like one unit of Continuing Education for listening to this episode, go to moderntherapistscommunity.com, purchase this course and pass the post test. A CE certificate will appear in your profile once you’ve successfully completed the steps.
Curt Widhalm 1:10:11
Once again, that’s moderntherapistscommunity.com.
Announcer 1:10:15
Thank you for listening to The Modern Therapist’s Survival Guide. Learn more about who we are and what we do at mtsgpodcast.com. You can also join us on Facebook and Twitter and please don’t forget to subscribe so you don’t miss any of our episodes.





SPEAK YOUR MIND